Getting the most out of each workout requires more than just following a great training
program. Consistent performance also requires an optimal balance between
training and recovery. Mention the subject to most clients, though, and you’re
likely to meet with disinterest or even resistance. Clients rarely think of
recovery as a planned activity, and others go so far as to believe that time
spent recovering will interfere with goal achievement.
So, in addition to all of our other roles as exercise experts, it’s up to us to help clients learn how and why to embrace recovery. Make sure recovery training is on your and your clients’ radar with this research review of its substantial benefits and the proper strategies for optimal recovery. Further, you’ll find a practical overview of how a recovery program can be integrated into the NASM Optimum Performance Training™ model.
Defining Recovery
Recovery relies on a reduction of, change in or break from stressors (Kellmann & Beckmann 2018). A more comprehensive definition of recovery is “an inter- and intraindividual multilevel (e.g., psychological, physiological, social) process in time for the re-establishment of personal resources and their full functional capacity” (Kallus & Kellmann 2016).
Exercise and training lead to tissue damage, inflammation, soreness and perceived fatigue (Dupuy et al. 2018). Kellmann et al. (2018) refer to this as “functional overreaching,” adding that it is required for performance enhancement but “can be compensated through comprehensive recovery.” These researchers go on to say that if recovery is not achieved, the athlete moves into a state of underrecovery, which serves as a precursor to overtraining syndrome.
Avoiding underrecovery begins by applying recovery strategies
systematically. Recovery strategies can be those activities that take place
either following a training session or between training sessions. Kellmann and
colleagues define such activities—whether passive (e.g., massage) or active
(e.g., postexercise cooldown)—as regeneration (Kellman et
al. 2018). Other recovery categories include sleep, nutrition and alleviation
of nervous system fatigue, as well as effective stress management skills, as it
is the culmination
of events that ultimately determine the body’s state of readiness.
Passive recovery techniques—such as massage, cryotherapy, compressive garments, water immersion and electrostimulation—are garnering a significant amount of evidence supporting their use as effective methods of recovery (Dupuy et al. 2018). As these strategies require either a license or expensive equipment, I won’t cover them here.
**Follow the link for a blog post and a great overview of passive recovery strategies.
Instead, I will focus on active recovery strategies—those that require the user to be an active participant—are the focus of this article.
Measuring Recovery
In research studies, the most common measures of recovery are markers of
performance (e.g., strength, power, speed) and soreness after a workout
(referred to as delayed-onset muscle soreness, or DOMS). A recovery method is
considered effective if it results in the user experiencing less soreness and
recovering baseline levels of strength and power more quickly.
It is important to recognize that while recovery techniques vary, they
share a similar purpose: facilitating the removal of metabolic waste (e.g.,
damaged proteins) from the muscle and allowing fresh nutrients to infiltrate
the area (Dupuy et al. 2018).
I would be remiss if I did not at least mention that lactic acid or
lactate production is likely not associated with muscle fatigue or
soreness and does not need to be “removed” or “flushed out.” As Len Kravitz,
PhD, points out, the burning sensation during exercises (i.e., acidosis) is a
result of the accumulation of protons in the cell. Lactate is produced in
response to this proton accumulation to help “neutralize or buffer the cell”
(Kravitz 2005). Therefore, lactate production is, in fact, a positive response
to intense exercise.
Active Recovery Strategies: Research and
Timing
Active regeneration strategies may be integrated immediately after a
training or exercise session (cooldown, stretching and myofascial rolling), or
they may be performed between sessions (low-intensity exercise). Let’s look at
when each strategy is intended to be performed, why the timing matters and what
support research offers.
Cardio
Cooldown (Immediately After)
While the common cooldown of 5–10 minutes of cardio post-exercise is
still one of the most popular methods of active recovery, there is little
evidence that it is superior to other types of recovery. In one study, Coffey,
Leveritt & Gill (2004) found that a traditional cooldown was the same as a
passive recovery after intense exercise. Similarly, when a 20-minute cycling
bout was performed at a moderate intensity (~70% of heart rate maximum) after
eccentric knee extensions (which induced DOMS), participants felt the same
level of discomfort as those in the low-intensity group (~30% of HRmax) (Tufano
et al. 2012). The researchers noted a reduction in DOMS in both groups at the
72- and 96-hour marks, which was likely due to natural causes and nothing to do
with the aerobic exercise.
The traditional cardio cooldown may provide the body with a smooth
transition from an exercise state back to a steady state, but the research does
not fully support a bout of light- or moderate-intensity aerobic exercise to
reduce the negative effects of DOMS. Therefore, it is not wrong to include
cardio as part of a cooldown, but know this may not be the key to
reducing DOMS.
Static
Stretching (Immediately After)
Stretching has been used to help prevent muscle imbalances by restoring
optimal muscle length. It is frequently touted as a way to prevent or reduce
the negative effects of DOMS. The research to support this notion is scarce.
However, stretching combined with other recovery strategies has proven to be
effective. Calleja-González et al. (2016) stated that massage combined with
stretching produced a positive effect on recovery when applied immediately
after a sports competition. But how can these results be replicated if an
individual cannot get a massage after each training session? Let’s explore the
use of myofascial rolling with the thought of it being a viable substitution.
Myofascial
Rolling (Immediately After)

The research on myofascial rolling has increased significantly over the
past 5 years. Such research has found that using roller massage as part of an
active recovery may help to speed up the recovery process (MacDonald et al.
2014; Wiewelhove et al. 2019). In a recent meta-analysis, Wiewelhove and
colleagues reviewed seven studies that explored the effects of post-exercise myofascial
rolling, and the researchers found that it reduced the perception of pain
caused by DOMS and, albeit slightly, helped to restore sprint and strength
performance. However, there is currently no evidence-based rationale for why
those who use roller massage experience a reduction in discomfort.
Hotfiel et al. (2019) highlighted that swelling via an accumulation of
interstitial fluid, as well as the presence of inflammatory substances, was
likely to blame for the pain with DOMS. It is reasonable to assume that the
direct compression and rolling help to move and potentially recirculate the
accumulated fluid, thus reducing the perception of pain. Further elaborating
this idea of post-exercise compression and DOMS, Beliard et al. (2015) and
Dupuy and colleagues explored compression garments used after exercise and
found that DOMS did indeed decrease.
Whether the positive results are due to flushing of inflammatory fluids
and metabolic waste or something else, such as a neurophysiological effect
occurring via a nervous system response, there appears to be support for using
roller massage as part of an integrated recovery strategy. It is important to
recognize that the use of myofascial rolling does not eliminate soreness but
may significantly reduce it. Therefore, returning to the question posed in the
section on stretching, it is possible that combining post-exercise myofascial
rolling with stretching may result in recovery benefits similar to those found
with massage plus stretching.
Low-Intensity
Exercise (Between Sessions)
In one thorough review, Cheung, Hume & Maxwell (2003) concluded that
low-intensity exercise was the most effective method of reducing soreness
between exercise sessions. It is important to recognize that such exercise is most
beneficial after
soreness is already present. Cheung, Hume & Maxwell included
that the individual should perform familiar total-body movements for 1–2 days
after the DOMS-inducing exercise.
It is speculated that the rhythmic contraction of muscles during
exercise may serve as an effective “pump” to mobilize inflammatory fluids that
are often associated with DOMS or to “warm up” the tissue, which may have a
temporary pain-reducing effect. However, there is far more evidence to suggest
that movement produces a pain reduction effect through complex cortical
processes. A study from the University of Iowa cites numerous studies that
demonstrate that exercise can reduce pain in people with knee replacements,
osteoarthritis and other chronic pain syndromes. It appears that exercise helps
to manage the central nervous system by inhibiting many of the pain-producing
mechanisms and reducing excitation (Lima, Abner & Sluka 2017).
The exercise used in such research is generally traditional aerobic
exercise, such as the use of a stationary bike or treadmill; however, this is
due to the ease of controlling the intensity and availability of such
equipment. Calisthenics—defined by Tsourlou et al. (2003) as exercises that
solely use one’s body weight—can help to significantly reduce pain in
conjunction with traditional therapy (Gurudut, Welling & Naik 2018).
Recovery Training With the NASM OPT™
Model
To summarize, the research points to the use of (1) myofascial rolling
and light stretching immediately after training, and (2) low-intensity,
total-body movement sessions between higher-intensity sessions.
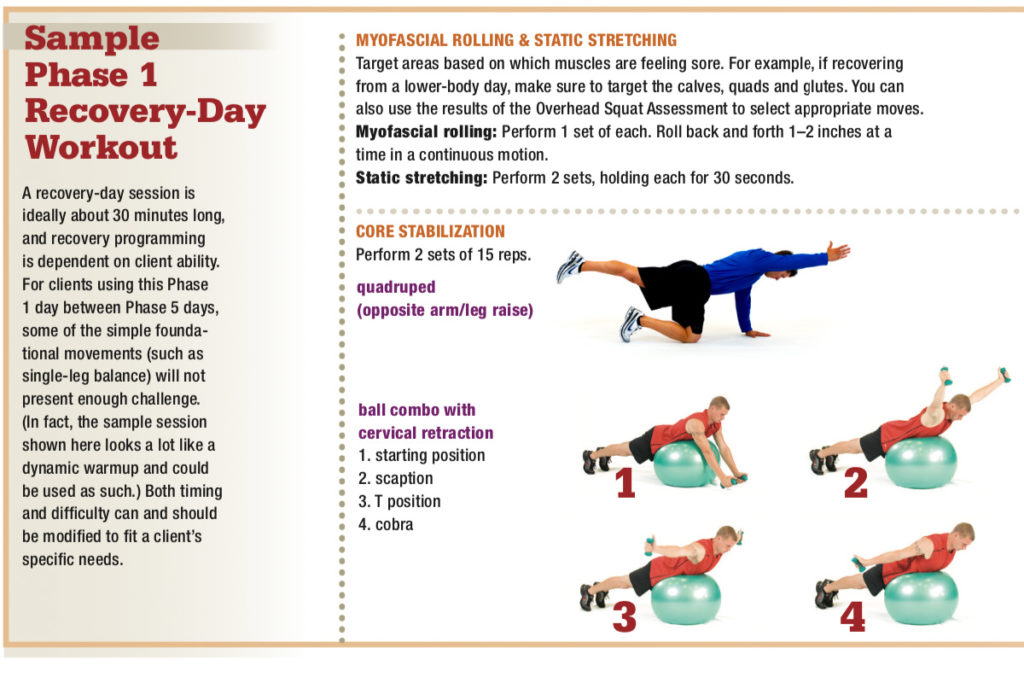
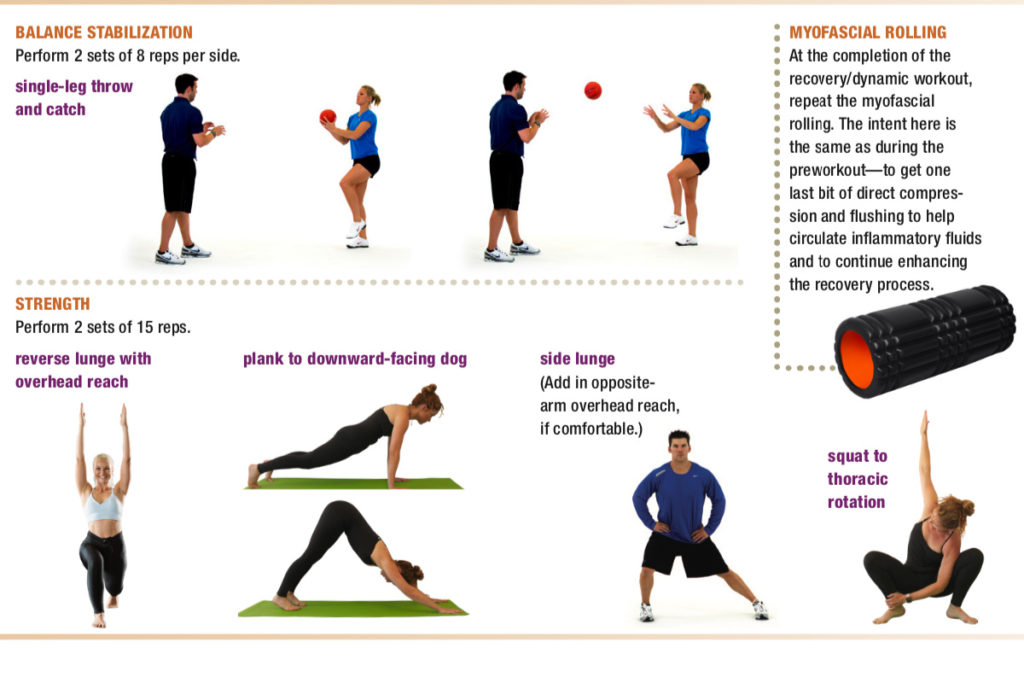
Using the NASM OPT model as a framework, a “recovery day” could include
a Phase 1: Stabilization Endurance workout planned 1–2 days after a Phase 3, 4
or 5 workout. This Phase 1 workout should be implemented according to NASM with
these exceptions:
SMR: When myofascial rolling, do not hold on tender spots.
Think of the rolling application as being a method of “flushing” the tissue. Roll back and forth in slow, continuous motion (1–2 inches per second for 30–60 seconds). Reserve the tactic of “holding pressure on one spot” for your pre-exercise rolling routine.
Plyometric and SAQ training: Avoid these.
Plyo and speed, agility and quickness (SAQ) exercises should be avoided due to the impact and the high levels of eccentric deceleration involved, which can exacerbate the discomfort associated with DOMS.
Body-weight moves: Emphasize mobility-enhancing exercises.
For example, instead of a regular lunge, add in an overhead reach (see “Sample Phase 1 Recovery-Day Workout,” below). These total-body mobility moves will do more than just encourage flexibility, as integrating more moving parts encourages a higher heart rate and an increase in overall tissue temperature.
Resistance moves: Modify the tempo.
More specifically, do not emphasize the eccentric phase of the exercise—have the client use smooth, coordinated and continuous movements. I know this sounds blasphemous to many hardcore NASM-ers, but the rhythmic contractions are helping to move fluid and metabolic waste through the sore tissues.
Reading Up on Recovery
Recovery and regeneration are hot topics for athletes and the general population, as well as for researchers. With the growing research and recovery technology, I encourage you to do a personal exploration of the field to determine what works best for your environment and with your clients. Learning as much as you can about recovery will allow you to provide more comprehensive service to every client. Being able to plan recovery sessions instead of merely recommending recovery will get your clients to their goals sooner and boost your business!
Specialize in Corrective Exercise
As a certified personal trainer, it’s important to realize that just about every client you work with may be susceptible to common injuries and ailments, ranging from lower-back pain to anterior cruciate ligament tears to shoulder pain. NASM’s Corrective Exercise Specialization applies to all clients, which means it lets you bring increased value to new and existing customers. Obtaining the NASM-CES demonstrates your continued passion and investment in education. Establish yourself as a fitness industry leader today.
[easy_media_download url="https://blog.nasm.org/wp-content/uploads/2019/10/AFM_Fall19_SM.pdf" text="Download the Fall 2019 Issue of the American Fitness Magazine" width="550" color="blue_four" target="_blank"]