Originally published in the spring 2019 issue of the American Fitness Magazine.
News flash! There’s a substance, available right now, that improves mood and cognition, reduces the risk of high blood pressure and high blood glucose, and possibly helps reduce body weight and overeating.
There’s even compelling evidence that regular consumption decreases the burden of heart and kidney disease and, in fact, makes all types of cells better at their jobs (while ensuring that they die when it’s their time to go).
Drum roll, please: It’s water. Yep, good old H2O. (Okay, so the photo was a bit of a spoiler.) Even for Nutrition Coaches who have always valued good hydration in their own self-care regimen, many of the associated complexities may come as a surprise, as they are grounded in research that is new or has been recently updated.
If you thought water was basic and boring, it’s time to look at it in a new light.
Are you ready to meet an old friend again for the first time? Go ahead and refill your water bottle first. I’ll wait.
It’s Not Just “Water In, Water Out”
Hydration. It seems like it should be pretty basic: Drink when you’re thirsty; pee when you have to go. You’re good. Right? Not quite.
 Previously viewed as a state (yes, no or almost), hydration might be better regarded as a process that includes an ongoing set of behaviors and biological functions. Determining a person’s hydration status is complex: It shifts repeatedly throughout the course of a day, so it’s not a steady state. Addressing hydration as a process makes sense because regular intake of fluids and excretion of urine, in and of themselves, confer benefits beyond maintaining water levels in the body (Lafontan 2014; Perrier et al. 2014).
Previously viewed as a state (yes, no or almost), hydration might be better regarded as a process that includes an ongoing set of behaviors and biological functions. Determining a person’s hydration status is complex: It shifts repeatedly throughout the course of a day, so it’s not a steady state. Addressing hydration as a process makes sense because regular intake of fluids and excretion of urine, in and of themselves, confer benefits beyond maintaining water levels in the body (Lafontan 2014; Perrier et al. 2014).
Drinking plenty of water is also an effective strategy for cutting weight!
Water: You Need It, Bad
Humans have an inherent, critical need for water. It is the medium in which all of our metabolic reactions occur. It gives form to our cells, lubricates our joints and tissues, transports nutrients and waste, and dissipates excess body heat (Horswill & Janas 2011; Lang 2007).
Not only is regular fluid intake (particularly plain water) one of the easiest, cheapest health interventions ever; it may also be one of the keys to optimizing health and well-being over the long term (Lang et al. 2017; Perrier 2017; Perrier et al. 2014). Good hydration habits appear to have an outsized positive impact on renal, cardiovascular and endocrine health and may even play an important role in addressing obesity (Chang et al. 2016; Perrier et al. 2014).
Read also: Recommended Daily Water Intake
For example, in a study of people diagnosed with overweight or obesity, those who consumed 500 milliliters of water just before each daily meal lost 2 kilograms more over the 12-week study than did those on the same diet who did not imbibe before each meal. It seems that drinking water before meals reduced energy intake, improving hydration and weight loss in a single step (Horswill & Janas 2011).
Finally, if that’s not enough to get you reaching for plain water, a recent study found that drinking 0.5 liter of water increased energy expenditure at rest by 30% for about 90 minutes (Horswill & Janas 2011)!
Water, by the Numbers
The amount of water in the body is referred to as total body water (TBW), and it represents 50%–60% of total body mass (or 70%–80% of fat-free body mass) (Horswill & Janas 2011).
TBW is in constant flux, with continual losses to respiration (as water vapor) and insensible sweat (perspiration that happens before it is perceived), as well as intermittent losses to urine, feces and sensible (perceived) sweat. This output is about 2.5 L/day, with additional losses occurring from physical exertion or a hot environment. Also variable (but more within an individual’s control) is the intake of fluids necessary to offset these losses. For most people, beverages account for about 60% of water intake, foods 30%. Metabolism contributes the final 10% as a byproduct of fat burning.
Water needs vary from person to person. For instance, people with obesity require more fluids than nonobese populations, owing to metabolic rate, body surface area and body weight (Chang et al. 2016). For context, however, the National Academy of Medicine (formerly the Institute of Medicine) says that adequate fluid intakes for male and female adults are 3.7 L/day and 2.7 L/day, respectively, with 0.7 L and 0.5 L of that coming from food (Kavouras & Anastasiou 2010). That’s a lot of fluid needed from beverages, and there is evidence that most Americans drink significantly less than this.
Worried about water weight? Don't be! Check out this blog on how to lose water weight effectively!
Dehydration versus hypohydration
If we stop thinking of hydration as a yes/no state, we can start considering the different levels of “almost” and why they matter. Technically speaking, dehydration is a 4% or greater drop in TBW, but a fluid loss as small as 2% of body mass will noticeably diminish both mental and physical function. Thanks to the adaptability of the human body, it’s fairly easy for people to walk around in a state of mild underhydration (a loss of 1%–3% of TBW)—referred to as hypohydration—without drastic day-to-day consequences. However, the acute adjustments that allow the body to compensate can also set us up for longer-term trouble.
Over the last decade or more, research has focused on the effects of chronic hypohydration and found that it may undermine overall health in ways big and small (Armstrong & Johnson 2018; Benelam & Wyness 2010; Enhörning et al. 2017; Horswill & Janas 2011). It can negatively affect mood, cognition, metabolism, and kidney and cardiac health, while possibly having implications for immune function and cancer prognosis (Benton et al. 2016; Enhörning & Melander 2018; Guelinckx et al. 2016; Melander 2016; Perrier 2017; Roumelioti et al. 2018). (More on consequences later.)
To really grasp how dehydration and hypohydration affect the body, it helps to look more closely at the physical processes involved. As with real estate, one of the first things to consider is location, location, location.
Water, Water—Everywhere
Most water in the body resides in two types of compartments: intracellular (within the cells) and extracellular (outside the cells). The two primary extracellular compartments are the intravascular compartment, which contains plasma (the fluid component of blood), and the interstitial compartment, which contains any fluid not located in the body’s cells or plasma. Intracellular fluid (ICF) refers to water inside cells, and extracellular fluid (ECF) refers to water outside of cells (in the interstitium or plasma).
Because cell membranes are permeable to fluid via aquaporins (specialized water channels), fluid moves freely between the three compartments (intracellular, intravascular and interstitial). One cause of this is osmosis: In osmosis, water moves from areas of high fluid concentration to areas of low concentration in an attempt to balance the levels on both sides of the cell membrane. This movement is driven, in part, by the quantity of solutes (substances dissolved in the fluid) in each compartment. Solutes cannot move through cell membranes, but fluid can. During osmosis, water moves from areas of lower solute concentration to areas of greater concentration, shifting the amount of water on each side of the membrane. An area with a higher solute concentration cannot help but pull water into it, even if this creates other problems.
When equilibrated, the three compartments—think of them as buckets—hold the appropriate amounts of fluid. However, when one bucket experiences a loss of water volume or an increase in solute concentration, water from another bucket is more likely to pour in to balance things out. This difference between solute concentrations on the two sides of a semipermeable membrane is called an osmotic gradient, and it drives water flow between compartments.
Water moving into or out of the ICF may cause cells to shrink or expand. A little change in size is a small problem, but large shifts can trigger undesirable signaling cascades affecting metabolism, transport, hormone release, cell proliferation and programmed cell death (Guelinckx et al. 2016; Lang 2007; Lang et al. 2017; Nishiyama & Kobori 2018). Cells get ticked when they shrink or swell. Shrinkage of cells in the ICF is the consequence of chronic hypohydration, and you will soon see why it has been accused of health crimes.
While the rules of osmosis may seem cut and dried (fluid shifts until balance is achieved), the body is more complex than that: Certain parts of the body do a more important job than others, so they take priority when it comes to allocation of resources, including water.
Case in point: Plasma accounts for only 7% of TBW, while most of the body’s water—about 60%–70%—is found in intracellular fluid. However, adequate blood volume is critical to maintaining whole-body homeostasis. Plasma is, after all, the body’s crucial transporter of nutrients, waste, oxygen and carbon dioxide. Viscous blood doesn’t flow as nicely and tends to clump. Lower blood volume (and thicker blood) means each organ system (heart, lungs, kidneys, liver, etc.) has to make do with less, making its job more difficult. Thus, the body prioritizes the intravascular compartment (containing plasma) at the expense of other fluid compartments.
 One demonstration of this prioritization is that blood osmolality—the balance of water to dissolved substances—remains remarkably consistent in people with widely different levels of habitual water intake. Thus, the intravascular compartment’s volume is maintained, but if enough fluid for this purpose is not provided by an external source (i.e., food or drink), the water has to come from somewhere within the body. This need can arise, for example, when “ad libitum” intake (fluid intake based on sensations of thirst or desire for liquid) is subject to “unconscious, involuntary dehydration,” where the individual drinks to satiety but does not overcome a water deficit (Stookey, Hamer & Killilea 2017).
One demonstration of this prioritization is that blood osmolality—the balance of water to dissolved substances—remains remarkably consistent in people with widely different levels of habitual water intake. Thus, the intravascular compartment’s volume is maintained, but if enough fluid for this purpose is not provided by an external source (i.e., food or drink), the water has to come from somewhere within the body. This need can arise, for example, when “ad libitum” intake (fluid intake based on sensations of thirst or desire for liquid) is subject to “unconscious, involuntary dehydration,” where the individual drinks to satiety but does not overcome a water deficit (Stookey, Hamer & Killilea 2017).
What About Electrolytes?
Maintenance of TBW depends not only on fluid ingestion but also on electrolyte concentration gradients in the fluid compartments. Electrolytes are electrically charged particles (anions or cations) from salts dissolved in water, and they are important for both rehydration (fluid replacement) and the capacity to hold onto a higher level of body water.
Predominant osmolytes in the ICF and ECF are the electrolytes potassium (K+) and sodium (Na+), respectively. Sodium exerts the strongest influence because of its role as primary driver of volume in the extracellular compartments (Leiper 2015).
This information is particularly important when working with endurance athletes, because Na+ is a primary component of sweat, and people with a faster sweat rate will lose more sodium in a given exercise session (Armstrong et al. 2010). Fluid to form sweat is drawn from blood plasma, so exercise of longer duration poses a challenge to blood volume and viscosity. As plasma volume decreases, its tonicity increases, thus pulling water out of the body’s cells.
Read also: Foods to Replenish Electrolytes:
Most diets in developed countries supply sufficient sodium to retain ingested water and, of note to athletes, to prevent exertional cramps. If you have clients on sodium-restricted diets, they should initiate a discussion with their physician: In 2013, the Institute of Medicine reported that there was a lack of conclusive scientific evidence of benefit (or harm) in reducing sodium consumption to previously recommended levels (Kong et al. 2016). If dietary Na+ is low or restricted, it may inhibit restoration and retention of ingested fluids, which can allow hypohydration to develop or continue. On the other hand, even athletes do not need excessive Na+ intake.
The Body’s Balancing Act
The body’s fluid-to-electrolyte balance—osmolality—is regulated by the renin-aldosterone-angiotensin system (RAAS). This controller, involving the brain, the kidneys and sensors throughout the body, is tasked with ensuring that we have enough Na+ to sustain cellular function and fluid balance. This, in turn, drives blood volume and therefore blood pressure.
When blood osmolality increases above normal (285–295 milliosmoles/kg, or mOsmol/kg), it is detected by osmoreceptors in the brain. This triggers the pituitary to release arginine vasopressin (formerly known as antidiuretic hormone). AVP triggers reabsorption of water by the kidneys, making urine more concentrated. It also results in constriction of blood vessels to maintain blood pressure and elicits feelings of thirst, inducing fluid intake.
In conjunction, pressure-sensitive receptors in blood vessels (called baroreceptors) sense the decreased blood volume and respond by triggering the release of aldosterone, a corticosteroid. Aldosterone increases Na+ reabsorption by the kidneys (and because water follows salt, this enhances water retention). Aldosterone also stimulates Na+ appetite, which further increases thirst (Boone & Deen 2008; Enhörning & Melander 2018; Kavouras & Anastasiou 2010; Roumelioti et al. 2018).
When blood osmolality decreases or there is a large influx of water from the small intestine, AVP drops, thirst disappears, and the kidneys produce a greater volume of dilute urine.
A Little Low on Water?
While occasional mild hypohydration is not a problem, being chronically dehydrated may be a threat to long-term health and well-being. Low TBW keeps the RAAS in a constant state of activity, with high circulating levels of the hormone cortisol. This suggests an overstimulation of the body’s stress response system.
In terms of exercise, fluid is important not just for aerobic performance but also for maintaining optimum muscle tissue. Dehydration leads to increased production of urea (a crystalline compound in urine), suggesting that water deprivation is accompanied by body tissue catabolism (breakdown). Chronic hypohydration appears to increase catabolism even when dietary protein needs are met (Kavouras & Anastasiou 2010; Lang et al. 2017; Stookey et al. 2013).
Also check out: Monitoring Hydration Levels
There is evidence that those with persistently low body water are at higher risk of serious chronic conditions, including type 2 diabetes, kidney disease and metabolic syndrome (abdominal obesity, insulin resistance, hypertension and persistent inflammation). AVP apparently alters liver glucose production and its breakdown of stored glycogen, while also impairing insulin secretion and insulin sensitivity (Qian 2018).
In people diagnosed with type 2 diabetes, low TBW deteriorates glucose regulation. Diabetes is already a challenge to TBW because excess glucose in the blood acts as an osmolyte, pulling water from cells to counteract the higher osmotic pressure in the ECF. The kidney glucose transporters become saturated, so glucose is lost in the urine, pulling excess water with it. Thus, the water never gets to the ICF, where the thirst was triggered—hence, the diabetes symptoms of excessive thirst (triggered by cellular dehydration) and large volumes of urine (following glucose loss in the urine). Although it may seem counterintuitive (given the excessive urine production), restricting water will only exacerbate the problem for people with diabetes. Blood glucose clearly needs to be controlled, but optimal hydration will help the body better manage the condition overall.
A broad range of other diseases are also associated with markers of hypohydration: heart failure, vascular dementia, cognitive impairment, inflammatory bowel disease, cancer and premature mortality (Lang et al. 2017). Obviously, many of these illnesses are multifactorial, and association is not causation.
 Nonetheless, those are heady concerns for a substance that, until recently, didn’t even figure into nutrition recommendations. Here’s the good news: Of all the ills associated with our underactive, overfed modern lives, hypohydration has an inexpensive, uncomplicated fix. In a 2016 study, people with low to moderate fluid intakes who increased their water consumption over as little as 6 weeks saw a nearly 25% drop in circulating copeptin, a marker of AVP associated with low TBW (Lemetais et al. 2017). Study participants consumed either 50%–80% or 80%–120% of fluid intake recommended by the European Food Safety Authority, and the results were similar for both groups.
Nonetheless, those are heady concerns for a substance that, until recently, didn’t even figure into nutrition recommendations. Here’s the good news: Of all the ills associated with our underactive, overfed modern lives, hypohydration has an inexpensive, uncomplicated fix. In a 2016 study, people with low to moderate fluid intakes who increased their water consumption over as little as 6 weeks saw a nearly 25% drop in circulating copeptin, a marker of AVP associated with low TBW (Lemetais et al. 2017). Study participants consumed either 50%–80% or 80%–120% of fluid intake recommended by the European Food Safety Authority, and the results were similar for both groups.
These recommendations are lower than those from the National Academy of Medicine. For adults, EFSA recommends water intakes of 2.5 L/day for men and 2.0 L/day for women—that’s 1.2 L and 0.7 L less, respectively, than the National Academy of Medicine suggests (EFSA 2017; Kavouras & Anastasiou 2010).
Soaking It Up
Many factors affect how quickly the body takes in fluids consumed in food and beverages. Water absorption, which occurs mainly in the small intestine, is important for everyone but may be particularly of interest to athletes wondering how much (and what) to drink before, during and after various levels of energy expenditure.
Whether we absorb the water from fluids we consume depends on our gastric emptying rate, or how fast fluid leaves the stomach. Gastric emptying rate is a function of several things, including the volume of fluid in the stomach, the calories in that fluid and the body’s immediate energy expenditure. Following are some factors to consider when seeking to speed up gastric emptying rate and get fluids to the body parts that need them most.
VOLUME AND TEMPERATURE
In general, the greater the volume of fluid in the stomach, the faster it exits. This is true up to about 600 mL, at which point the rate may level off. Personal tolerance varies, of course. (Many athletes have learned the hard way that a competition or major event is not the time to test one’s limits!) Interestingly, refilling the stomach regularly with a larger volume, rather than drinking slowly and continually, will enhance gastric emptying (Leiper 2015); however, drinking a large volume in a short time right after working out is not recommended.
Beverage temperature, contrary to a popular myth, does not affect water uptake. Cold drinks are often the most palatable in an exercise situation, particularly in a hot environment, so it’s good to know temperature will not slow the rate of gastric emptying or intestinal absorption (Leiper 2015).
CALORIES AND ELECTROLYTES
Plain water is emptied from the stomach and absorbed in the intestine faster than fluids containing electrolytes or calories. But even large doses of fluids with electrolytes or calories are likely to be rapidly filtered, as the body’s regulation system may perceive a water overload. Here are a few types of beverages and their notable characteristics:
FRUIT JUICE AND SOFT DRINKS. Solute concentration in fluids (osmolality) is measured in milliosmoles per kilograms. In beverages with similar energy and electrolyte contents, a moderately hypotonic solution (229 mOsmol/kg) is absorbed two times faster than an isotonic (277 mOsmol/kg) or moderately hypertonic (352 mOsmol/kg) solution. The problem with hypertonic beverages, which include fruit juice and soft drinks, is that they draw water out of the body-water pool into the intestine to make them isotonic; this delays absorption of their water content and makes them ineffective for rapid rehydration, especially during or following competition (Leiper 2015).
SPORTS DRINKS. Carbohydrate-electrolyte solutions (aka sports drinks) that have a carbohydrate concentration of 2.5% or less will empty from the stomach about as fast as plain water. However, sports drinks can have their problems. Those with carbohydrate concentrations of 6% or higher will slow gastric emptying and may cause GI distress during activity (Leiper 2015; Maughan & Leiper 1999). Also, many store-bought versions contain fructose, which has been shown to enhance carbohydrate oxidation at low-to-moderate exercise intensities but can be difficult for some people to digest (Jeukendrup 2017).
(Incidentally, fructose is found in fruit juices and many other sweetened beverages, too.) If someone gets gassy or uncomfortable after drinking a commercial sports drink, fructose may be the culprit. Fortunately, a sports drink can be made at home to suit an athlete’s precise tastes and needs, at a low cost.
CAFFEINE. Although caffeine has an acute, mild diuretic effect (spurring production of excess urine), it is not dehydrating when consumed in levels below 500–600 milligrams/day. (For context, a Starbucks 12-ounce black coffee has about 240 mg, a double espresso about 160 mg.) Higher caffeine consumption can generate urine in excess of fluid intake, in which case additional fluid should be consumed to counteract this effect (Benelam & Wyness 2010).
Drinking Up, Working Out
 When exercise will last longer than 2 hours or take place in high heat, exercisers should arrive optimally hydrated—neither hyperhydrated (with an excess of TBW) nor hypohydrated (at a deficit). This is particularly important if fluid loss from sweat will be high (in which case sodium losses via sweat will probably also be high). Known as euhydration, optimal hydration likely improves anaerobic performance and certainly won’t hurt it, which cannot be said for taking in too much or too little fluid.
When exercise will last longer than 2 hours or take place in high heat, exercisers should arrive optimally hydrated—neither hyperhydrated (with an excess of TBW) nor hypohydrated (at a deficit). This is particularly important if fluid loss from sweat will be high (in which case sodium losses via sweat will probably also be high). Known as euhydration, optimal hydration likely improves anaerobic performance and certainly won’t hurt it, which cannot be said for taking in too much or too little fluid.
STARTING AT A LOSS
Beginning an endurance event hypohydrated compromises performance: The water deficit increases cardiovascular strain, raises heart rate and rating of perceived exertion for the same relative effort, and amplifies the thirst sensation. High temperatures increase the degree of impairment and discomfort. Using diuretics (which pull water from the ECF volume) to “make weight” in sports like wrestling and rowing, incurs greater strain during the exercise that follows (Cotter et al. 2014; James et al. 2017).
Dehydration, especially when it exceeds a loss of 2% body mass, reduces endurance exercise performance and shortens time to exhaustion (Armstrong et al. 2007). Anaerobic endurance, muscle strength and power all decrease, as well. Further, such dehydration can induce plasma hyperosmolality, which increases heat storage by delaying and decreasing sweating in an attempt to conserve water (Paull et al. 2016). Performance is more severely affected at fluid losses of 3%–4% of body weight. Therefore, as much as possible, body mass losses during an event should be limited to 1%–2%, and sodium should be included in fluids consumed (Shirreffs 2008).
In cooler temperatures, dehydration of more than 2% may be tolerable, but as the temperature increases, smaller levels of dehydration may have a greater effect. When continuous exercise is performed in heat, fluid intake exerts a greater magnitude of improvement (Shirreffs 2008; McCartney, Desbrow & Irwin 2017).
The dangers of overhydration
Overhydration does not enhance performance, either. Hyperhydration (higher than optimal TBW) does not improve aerobic or anaerobic performance and can, at extremes, be fatal (McDermott et al. 2017). Attempting to “stuff” fluids (especially plain water) beyond thirst can bring on a life-threatening condition called exertional hyponatremia.
The “na” in “hyponatremia” refers to sodium’s periodic table symbol, Na+. If blood levels of sodium become hypotonic (too dilute), osmotic pressure in the extracellular compartments decreases. Remember that sodium is the primary driver of ECF volume, so its loss or insufficiency means water will flow out of the ECF, further depleting volume, and will flow into the body’s cells, causing them to swell. This becomes particularly dangerous in the brain because cell swelling there will lead to increased intracranial pressure, a dangerous condition called cerebral encephalopathy. Exercise also results in the shunting of blood to active muscles, leading to decreases in kidney filtration and urine production and making it harder for the body to counter a fluid overload. Even with Na+ supplementation, exertional hyponatremia can occur, particularly in ultra-endurance events, or those lasting longer than 18 hours.
Because a lower TBW is more easily diluted, women are at higher risk of hyponatremia (Almond et al. 2005), as are people whose initial Na+ levels are low (owing to dietary restrictions, for example). Event duration is another risk factor: The longer it takes athletes to complete a marathon- or Ironman®-distance event, the more opportunity they have to consume excessive fluid, and the longer they will be sweating (and therefore losing Na+). Use of medications such as nonsteroidal anti-inflammatory drugs (NSAIDs) and selective serotonin reuptake inhibitors (SSRIs) confer additional risk (Cotter et al. 2014; Hoffman, Bross & Hamilton 2016). Clients may benefit from being made aware of the potential effects of these common medications.h
If you are overhydrating as a result of rhabdomyolysis, see a professional!
SWEATING THE SMALL STUFF
Average sweat rate can help you roughly determine fluid losses, as can simple strategies for checking hydration (see “How to Calculate Sweat Rate,” above). Looking at individual losses is important because sweat rate ranges from 0.5 L/hour to extremes of 3.5 L/hour.
This does not mean you should attempt to consume that amount of fluid during each hour of exercise; it is unlikely you could absorb that much, and overhydration puts you at risk of exertional hyponatremia. Additionally, while negative consequences can ensue from drinking too much before or during exercise, consuming large amounts of fluid over a short time post workout is not advisable, either. This practice will overstimulate the kidneys, producing large volumes of urine, which undermines rehydration (Jones et al. 2010).
 Here’s an example of how to gauge rehydration needs: If your sweat rate is 2 L/hour and you consume about 1.5 L/hour, you’ll lose about 0.5 kg/hour over your intake, so after 3 hours you will have lost 1.5 kg, or about 2%. If you are able to absorb more than 1.5 L/hour (without feeling fluid sloshing in your stomach), you can try that.
Here’s an example of how to gauge rehydration needs: If your sweat rate is 2 L/hour and you consume about 1.5 L/hour, you’ll lose about 0.5 kg/hour over your intake, so after 3 hours you will have lost 1.5 kg, or about 2%. If you are able to absorb more than 1.5 L/hour (without feeling fluid sloshing in your stomach), you can try that.
It’s important to remember that it doesn’t take much overdrinking to overwhelm body Na+ stores. Generally speaking, the best strategy is to drink to thirst or comfort, but not beyond. If water is sloshing in your stomach, you don’t need to drink more.
Remember that heat factors into getting properly hydrated as well!
Getting It Back
Following dehydrating events or practices, rehydration is a process that occurs over time and requires ingestion of 150% of the volume lost to sweat. In situations when complete rehydration between events (particularly those of longer duration) is limited by time or availability, athletes should consume fluid as they can and then restore full TBW when possible (overnight, for example). In such cases, sports drinks can aid in replenishing electrolytes and carbohydrates as well as fluids (Leiper 2015; Shirreffs 2008).
A strategy of “metered” fluid consumption can help the process: This refers to dividing up the total fluid to be ingested into eight portions, the first to be consumed immediately after the event, with another dose every 30 minutes thereafter, until the process is complete. Metered consumption increases hydration efficiency—the amount of water retained by the body—without prolonging dehydration.
Of course, post workout is not the only time when it is important to counter dehydration. If your self-checks indicate dehydration at any time, increase your water intake by about 1.5 L (beyond what you normally drink) during the day. Your urine should be about two shades lighter within about 24 hours (Perrier et al. 2015), a good indicator that you’re back on track. This may be a topic to discuss with clients, too, as some may be experiencing chronic hypohydration and not be aware of it.
Show What You Know
Euhydration is not magic, but it’s a goal that can reverberate through one’s personal health and fitness. Barring medical contraindication, striving for consistent adequate intake of plain water can only enhance health now and in future years.
As fitness professionals, we provide all kinds of lifestyle improvement suggestions to our clients and gym members. Advising them of ideal hydration habits is another service we can provide that will enhance health. Further, the recommendations are simple and inexpensive, so barriers to improving hydration (other than the inconvenience of frequent urination) are typically low. In fact, drinking more water may be one of the easiest things you’ve ever suggested, with an outsized payoff for you and your clients, families and friends.
As always, our suggestions are most powerful when we model them, so hydrate thyself—and then help others soak up some knowledge, too.
glossary of hydration terms
dehydration: a loss of 4% or more of total body water (TBW); also the process by which body water is lost
diuretic: spurring extra urine production by kidneys to maintain TBW balance; a substance causing this effect
electrolyte: an electrically charged particle (anion or cation) resulting from salts dissolved in water
euhydration: the ideal amount of body water; necessary to sustain normal physiological functions of the body
extracellular fluid: fluid outside the body’s cells; includes fluid in the intravascular compartment (plasma, the fluid component of blood) and fluid in the interstitial compartment (not plasma and not fluid inside cells)
hyperhydration: an excess of TBW
hypohydration: a mild deficit of TBW (loss of 1%–3%)
hyponatremia: water toxicity; decreased concentration of Na+ in the body, due to overconsumption of fluid or a failure to spontaneously remove urine
intracellular fluid: fluid inside the cells
osmolality: the body’s water-to-electrolyte balance, measured in milliosmoles of solute per kilogram of solvent (mOsmol/kg)
osmolyte: a substance that affects the flow of fluids via osmosis
osmotic gradient: the difference in concentration between two solutions on either side of a semipermeable membrane
overhydration: excess fluid consumption, leading to excess TBW
rehydration: the process of restoring normal TBW from a hypo- or dehydrated state
tonicity: effective osmotic gradient; relative concentration of solutes; drives movement of water between body compartments
- hypertonic: more solutes outside the cell than inside
- hypotonic: more solutes inside the cell than outside
- isotonic: equal tonicity/relative osmotic pressure
total body water: the overall amount of water in the body
Special Considerations for Senior Populations
In people over the age of 65, TBW decreases. This is partly because water is dependent on fat-free mass, so age-related muscle loss, known as sarcopenia, causes TBW levels to drop. Osmo- and baroreceptors also become less sensitive in older adults, so thirst tends to be less pronounced and the kidneys become less effective at concentrating urine. For these reasons, determining hydration status becomes more difficult in seniors than in younger age groups (Armstrong & Johnson 2018; Guelinckx et al. 2016; Kavouras & Anastasiou 2010; Roumelioti et al. 2018).
For more information on the special needs of seniors, the NASM Senior Fitness Specialization provides guidance on fitness programming using the NASM Optimum Performance Training™ model, as well as understanding this group’s concerns, common conditions and fitness obstacles.
Easy Ways to Check Hydration—Without Lab Work
There are several ways to gauge hydration levels without doing lab work: They involve measures that are easy to check at home, including thirst, body weight, and urine volume and color.
THINK ABOUT THIRST
First thing in the morning, before exercising and before eating or drinking anything, assess your thirst on a scale of 1–9 (with 1 being “not thirsty at all” and 9 being “thirstiest I’ve ever been”). If you feel “very thirsty,” chances are good that you are down about 2% of body weight, meaning you’re mildly dehydrated. This thirst perception rating can serve as a good baseline throughout the day (Armstrong et al. 2014).
STEP ON A SCALE
Unless you are actively losing or gaining weight, most day-to-day variations in weight are from fluctuations in total body water. To establish a baseline, weigh yourself nude, first thing in the morning after using the bathroom, 3 days in a row. The average of these three weights is a pretty good representation of your weight. Keep a record of this number and use it for comparison with your postworkout weight. Then rehydrate accordingly.
Caveat: This is not a good gauge in the days after a high salt intake, which will cause fluid retention that does not correspond with good hydration. A sudden excess of water is eliminated very rapidly, within hours of consumption, but excess sodium takes days to be removed, demonstrating that these mechanisms operate on different time frames (Bie & Evans 2016).
CONSIDER YOUR OUTPUT
No one expects you to measure urine output (though you can if you want to), but if you don’t need to urinate at least every 3 hours or so, you probably aren’t euhydrated. Urine color can also help you assess your hydration level. A pale-yellow color indicates good hydration, and a darker, sunflower-yellow color shows normal hydration or slight dehydration. If the color shifts to a mustardy or brownish color, you are exhibiting a sign of dehydration (see the color chart below).
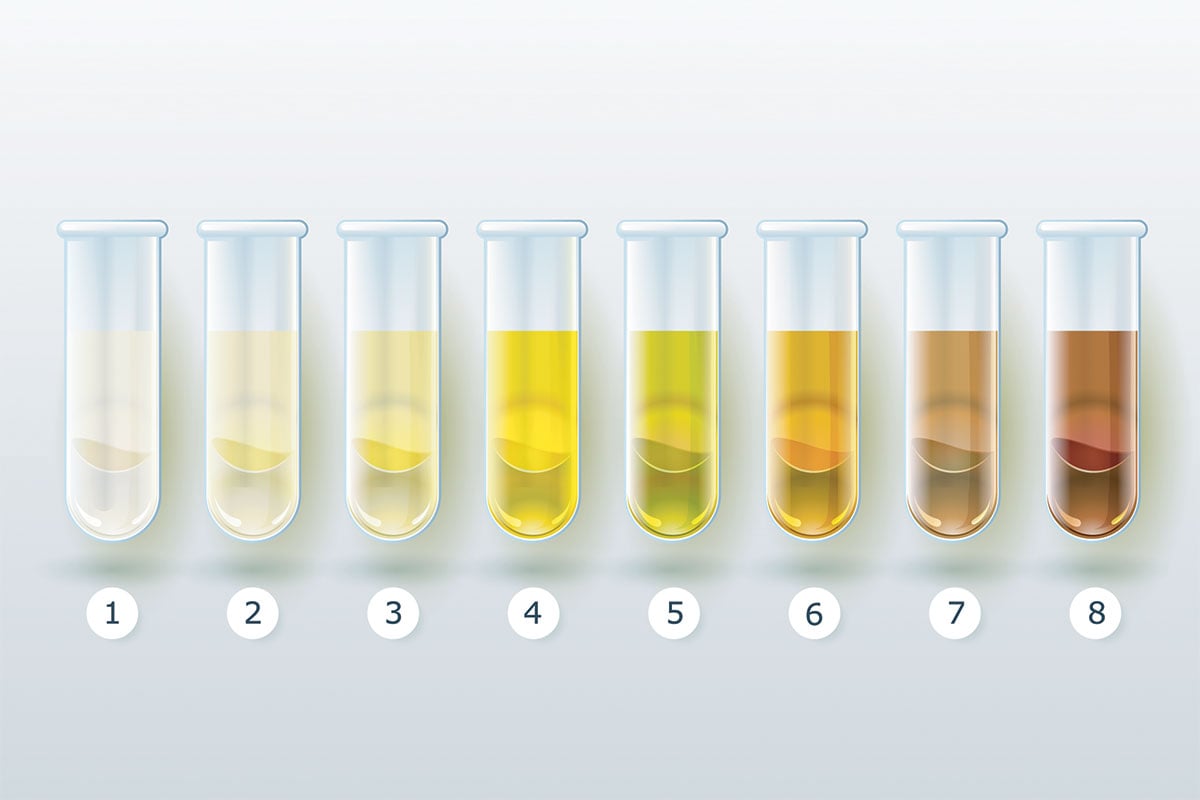
Caveat: Many things can affect urine color, including drinking a large quantity of water soon before urinating (which can lighten it) or taking B vitamins (which can darken it). Using at least two methods to gauge hydration will give you a clearer picture of where you stand.
How to Calculate Sweat Rate
Knowing how much water you lose to sweat can be helpful in sustaining hydration or at least in not losing too much fluid during a practice or event. It will also help you restore euhydration later. Here is an assessment that can help you approximate your average sweat rate (SR).
 THE 30-MINUTE SWEAT RATE TEST
THE 30-MINUTE SWEAT RATE TEST
- Empty the bladder, then take a nude weight (ideally in kilograms).Exercise for 30 minutes.Take a nude weight again.Subtract postexercise weight from pre-exercise weight, then double the difference to approximate SR per hour, in liters.
Note: The 30-minute test is easiest if you avoid eating or drinking anything during the exercise. If you drink any fluids beforehand, add that amount to the difference in weights in step 4.
Example: If your pre-exercise weight was 72 kg and you weigh 71 kg afterward, and you did not drink anything before the workout, your SR is 2 L/hour. If the weight difference is 500 grams and you drank 250 mL of fluid beforehand, add that to the 500 g for a loss of 750 g, or an SR of 1.5 L/hour.
REFERENCES
Almond, C.S.D., et al. 2005. Hyponatremia among runners in the Boston Marathon. The New England Journal of Medicine, 352, 1550–56.
Armstrong, L.E., & Johnson, E.C. 2018. Water intake, water balance, and the elusive daily water requirement. Nutrients, 10 (1928).
Armstrong, L.E., et al. 2007. Exertional heat illness during training and competition. Medicine & Science in Sports & Exercise, 39 (3), 556–72.
Armstrong, L.E., et al. 2010. Accumulation of 2H2O in plasma and eccrine sweat during exercise-heat stress. European Journal of Applied Physiology, 108 (3), 477–82.
Armstrong, L.E., et al. 2014. Novel hydration assessment techniques employing thirst and a water intake challenge in healthy men. Applied Physiology, Nutrition, and Metabolism, 39 (2), 138–44.
Benelam, B., & Wyness, L. 2010. Hydration and health: A review. Nutrition Bulletin, 35 (1), 3–25.
Benton, D., et al. 2016. Minor degree of hypohydration adversely influences cognition: A mediator analysis. American Journal of Clinical Nutrition, 104 (3), 603–12.
Bie, P., & Evans, R.G. 2016. Normotension, hypertension and body fluid regulation: Brain and kidney. Acta Physiologica, 219 (1), 288–304.
Boone, M., & Deen, P.M.T. 2008. Physiology and pathophysiology of the vasopressin-regulated renal water reabsorption. Pflügers Archiv—European Journal of Physiology, 456, 1005–24.
Chang, T., et al. 2016. Inadequate hydration, BMI, and obesity among US adults: NHANES 2009–2012. Annals of Family Medicine, 14 (4), 320–24.
Cotter, J.D., et al. 2014. Are we being drowned in hydration advice? Thirsty for more? Extreme Physiology & Medicine, 3 (18).
EFSA (European Food Safety Authority). 2017. Dietary reference values for nutrients: Summary report. Accessed Feb. 6, 2019: efsa.europa.eu/sites/default/files/2017_09_DRVs_summary_report.pdf.
Enhörning, S., & Melander, O. 2018. The vasopressin system in the risk of diabetes and cardiorenal disease, and hydration as a potential lifestyle intervention. Annals of Nutrition & Metabolism, 72 (2, Suppl.), 21–27.
Enhörning, S., et al. 2017. Effects of hydration on plasma copeptin, glycemia and gluco-regulatory hormones: A water intervention in humans. European Journal of Nutrition, doi.org/10.1007/s00394-017-1595-8.
Guelinckx, I., et al. 2016. Fluid intake and vasopressin: Connecting the dots. Annals of Nutrition & Metabolism, 68 (2, Suppl.), 6–11.
Hoffman, M.D., Bross, T.L., & Hamilton, R.T. 2016. Are we being drowned by overhydration advice on the internet? The Physician and Sportsmedicine, 44 (4), 343–48.
Horswill, C.A., & Janas, L.M. 2011. Hydration and health. American Journal of Lifestyle Medicine, 5 (4), 304–15.
James, L.J., et al. 2017. Hypohydration impairs endurance performance: A blinded study. Physiological Reports, 5 (12), e13315.
Jeukendrup, A.E. 2017. Periodized nutrition for athletes. Sports Medicine, 47 (1, Suppl.), 51–63.
Jones, E.J., et al. 2010. Effects of metered versus bolus water consumption on urine production and rehydration. International Journal of Sport Nutrition and Exercise Metabolism, 20 (2), 139–44.
Kavouras, S.A., & Anastasiou, C.A. 2010. Water physiology: Essentiality, metabolism, and health implications. Nutrition Today, 45 (6), S27–32.
Kong, Y., et al. 2016. Sodium and its role in cardiovascular disease—the debate continues. Frontiers in Endocrinology, 7, 164.
Lafontan, M. 2014. H4H—hydration for health. Obesity Facts, 7 (2, Suppl.), 1–5.
Lafontan, M., et al. 2015. Opportunities for intervention strategies for weight management: Global actions on fluid intake patterns. Obesity Facts, 8, 54–76.
Lang, F. 2007. Mechanisms and significance of cell volume regulation. Journal of the American College of Nutrition, 26 (5), 613S–23S.
Lang, F., et al. 2017. Two liters a day keep the doctor away? Considerations on the pathophysiology of suboptimal fluid intake in the common population. Kidney & Blood Pressure Research, 42, 483–94.
Leiper, J.B. 2015. Fate of ingested fluids: Factors affecting gastric emptying and intestinal absorption of beverages in humans. Nutrition Reviews, 73 (2, Suppl.), 57–72.
Lemetais, G., et al. 2018. Effect of increased water intake on plasma copeptin in healthy adults. European Journal of Nutrition, 57 (5), 1883–90.
Maughan, R.J., & Leiper, J.B. 1999. Limitations to fluid replacement during exercise. Canadian Journal of Applied Physiology, 24 (2), 173–87.
McCartney, D., Desbrow, B., & Irwin, C. 2017. The effect of fluid intake following dehydration on subsequent athletic and cognitive performance: A systematic review and meta-analysis. Sports Medicine—Open, 3, 13.
McDermott, B.P., et al. 2017. National Athletic Trainers’ Association position statement: Fluid replacement for the physically active. Journal of Athletic Training, 52 (9), 877–95.
Melander, O. 2016. Vasopressin, from regulator to disease predictor for diabetes and cardiometabolic risk. Annals of Nutrition & Metabolism, 68 (2, Suppl.), 24–28.
Nishiyama, A., & Kobori, H. 2018. Independent regulation of renin–angiotensin–aldosterone system in the kidney. Clinical and Experimental Nephrology, 22 (6), 1231–39.
Paull, G., et al. 2016. The effect of plasma osmolality and baroreceptor loading status on postexercise heat loss responses. American Journal of Physiology: Regulatory, Integrative and Comparative Physiology, 310 (6), R522–31.
Perrier, E.T. 2017. Shifting focus: From hydration for performance to hydration for health. Annals of Nutrition & Metabolism, 70 (1, Suppl.), 4–12.
Perrier, E.T., et al. 2014. From state to process: Defining hydration. Obesity Facts, 7 (2, Suppl.), 6–12.
Perrier, E.T., et al. 2015. Urine colour change as an indicator of change in daily water intake: A quantitative analysis. European Journal of Nutrition, 55 (5), 1943–49.
Qian, Q. 2018. Dietary influence on body fluid acid-base and volume balance: The deleterious “norm” furthers and cloaks subclinical pathophysiology. Nutrients, 10 (6), 778.
Roumelioti, M.E., et al. 2018. Fluid balance concepts in medicine: Principles and practice. World Journal of Nephrology, 7 (1).
Shirreffs, S.M. 2008. Symposium on ‘performance, exercise and health’ hydration, fluids and performance: Conference on ‘Multidisciplinary approaches to nutritional problems.’ Proceedings of the Nutrition Society, 68 (1), 17–22.
Stookey, J.D., Hamer, J., & Killilea, D.W. 2017. Change in hydration indices associated with an increase in total water intake of more than 0.5 L/day, sustained over 4 weeks, in healthy young men with initial total water intake below 2 L/day. Physiological Reports, 5 (22), e13356.
Stookey, J.D., et al. 2013. RBC deformability and amino acid concentrations after hypoosmotic challenge may reflect chronic cell hydration status in healthy young men. Physiological Reports, 1 (5), e00117.