Vu Nguyen was strong and fit. He didn’t drink or smoke. But on a sweltering July day in 2018, the 50-year-old Cleveland police officer collapsed during a 1.5-mile run that was part of a training exercise.
He died 4 days later. Medical authorities blamed rhabdomyolysis, a rare but
serious medical disorder that can result from overexercising (Hein 2018). In
another incident that grabbed headlines, the Paralympics snowboarder Amy Purdy
issued a plea to friends and fans from her hospital bed: “You have to listen to
your body. When it is telling you to stop, stop!” Purdy, a double amputee who
also competed on Dancing With the Stars, pushed too hard doing pullup
sets while training for the 2016–2017 snowboarding season. She was sore for a
day then noticed swelling in one arm, which sent up a red flag. She knew about
rhabdomyolysis because it had landed a friend of hers in the hospital the year
before. Purdy survived, but it was a long and occasionally painful recovery
(Mateo 2018).
I’ve been warning fitness professionals about the risks of rhabdomyolysis—or
“rhabdo,” as some of us call it—for more than a decade. While athletes and
fitness enthusiasts who engage in high-intensity exercise are the more obvious
candidates for rhabdo, it can also happen to novices and people trying an
activity they haven’t done before. Since veterans and newcomers alike are
vulnerable to the disorder, fitness pros need to understand the causes,
symptoms and tactics for prevention. This brief overview will give you the
basics.
Rhabdomyolysis: The Fundamentals
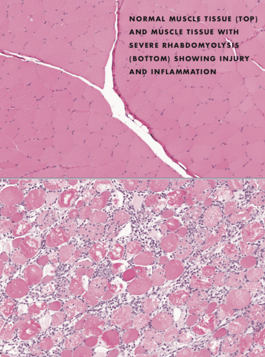
Rhabdomyolysis (rab-doe-my-OH-li-sis) occurs when striated muscle fibers rupture, releasing their contents into the bloodstream. This can have serious consequences that may require
hospitalization.
Rhabdo can result from a variety of conditions, including blunt trauma, surgery,
burns, drug and alcohol abuse, poisoning, electrocution, infections, and even
some medications. When exercise triggers the disorder, we call it exertional
rhabdomyolysis or exercise-induced rhabdomyolysis (Kim et al. 2016).
Some evidence hints that exertional rhabdomyolysis may be on the rise (Knafl et
al. 2018), though we don’t know for sure how often it occurs.
Causes of Exertional Rhabdomyolysis
The condition usually follows engagement in high-volume, high-repetition, intense or unfamiliar exercises or activities. Exercising in the heat and pushing beyond one’s physical capabilities can play
roles in rhabdo.
The biochemical mechanism of exertional rhabdomyolysis is not fully understood (Kim et al. 2016). It is thought that intense activity significantly depletes adenosine triphosphate (ATP) levels faster than they can be restored. This causes dysregulation of cellular sodium, potassium and calcium concentration and an increase in free radical production. Ultimately, this leads to a
breakdown in cytoskeletal membrane integrity, allowing cellular components to
enter the blood.
Symptoms, Risks, Incidence
Fitness professionals should not underestimate the hazards of rhabdo, which can cause many risky conditions and symptoms:
- heart rhythm abnormalities and heart attacks
- kidney failure
- severe muscle pain
- muscle weakness, swelling and bruising
- elevated liver enzymes
(Tsuruda et al. 2017; Keltz, Khan & Mann 2014; Scalco et al. 2016; Vucicevic 2015;
Tibana et al. 2018)
Brown Urine
Fitness pros may have heard about one rhabdo symptom: dark-colored urine, often described as looking like iced tea or cola.
The color change happens because high levels of the muscle protein myoglobin
get into the urine during the kidneys’ blood-filtering process.
Excessive myoglobin is toxic to the kidneys and can cause kidney failure. Indeed, some people may require dialysis to protect against kidney damage. Note that while darkened urine is the best-known symptom of rhabdo, it doesn’t happen to
everyone with the condition.
Muscle Swelling
Many people with rhabdo report swelling of the muscles used in the activity they were doing. The medical term is compartment syndrome, which results from increased fluid pressure inside muscles after an injury or physical trauma (which can be caused by overexertion).
This swelling is not like the temporary “pump” some gym-goers look for after
exercise.
Compartment syndrome is serious and painful because it can cut off blood supply to muscles. It can also cause muscle weakness and an inability to bend or extend limbs.
Some people have reported being unable to fit into clothing because of the
swelling. Sometimes, surgery is required to relieve the pressure.
Incidence
The incidence of rhabdo in the general population is not well-known. Most reports do not get published by clinicians. Some individuals who develop the condition never go to the hospital, further reducing the number of cases reported.
Literature reviews usually quote 26,000 cases each year from all causes, many of which are attributed to exercise (Sauret, Marinides & Wang 2002). Unfortunately,
these statistics date to the 1990s. More recent data on the prevalence of
exercise-induced rhabdomyolysis in the general population cannot be located.
Patient Profile
Much of what we know about exercise-induced
rhabdomyolysis comes from reports of hospital admissions. These reports have
documented rhabdo in many different groups:

- marathon runners
- elementary school students
- police academy cadets
- soldiers in training
- hikers
- bodybuilders
- high school gymnasts and wrestlers
- group exercise class participants
- college swimmers and football players
- people who were gardening
(Abbas et al. 2019; Clarkson & Eichner 2006; CDC 1990; Atias-Varon et al. 2017;
Pattison et al. 1988; Do, Bellabarba & Bhananker 2007; Lin et al. 2005;
Cannon 2017; Stanfa et al. 2017; Thompson, Nguyen & Karodeh 2018;
Vucicevic 2015; Cleary et al. 2011; Chen et al. 2013).
As this list suggests, exertional rhabdomyolysis can occur in both fit and unfit
individuals. Though high-profile rhabdo cases occasionally make it into news
media reports, I suspect that a large number of instances go undocumented. Do a
quick check on #rhabdo on your favorite social media channels and see for
yourself.
Exercise Intensity
Exercise intensity seems to increase the risk of rhabdo, and it’s important to remember that activities which don’t seem intense to fitness professionals may seem so to clients at a lower fitness level.
That said, intensity is not the only factor. In some people, activities not
considered intense can initiate the disorder. For example, one report noted
that a 29-year-old man developed rhabdomyolysis in his abdominals after
performing 30–40 situps a day for just 5 days (Kao et al. 1998).
The man in this report said he was a novice and not accustomed to exercise. In another report, a 55-year-old man developed rhabdomyolysis and kidney failure after gardening for several hours (Vucicevic 2015).

These reports highlight an often-missed aspect of exertional rhabdomyolysis: It appears to erupt after exercises and activities that people are not accustomed to doing. For personal trainers—whose clients are often novices—this is an important point to keep in mind.
In summary, the risk of rhabdomyolysis generally increases with the intensity,
volume, repetitiveness and novelty of the activity or exercise.
Diagnosis
Medical professionals have many ways to determine if someone has rhabdo, including checking for muscle swelling, weakness and pain and taking a detailed health history.
Physicians often test for elevated levels of an enzyme called creatine
kinase (CK), also known as creatine phosphokinase (CPK) (Keltz, Khan
& Mann 2014). CK can be a marker of muscle damage.
While exercise can raise CK levels, rhabdo can push them to more than 10 times higher than normal. Don’t be surprised if your post-rhabdo clients tell you how high their CK levels rose.
Doctors also test for myoglobinuria—the presence of myoglobin in the urine
(Keltz, Khan & Mann 2014). Tests scan for electrolyte imbalances and
elevated liver enzymes, as well. Thus, there is more to diagnosing rhabdo than
the color of someone’s urine.
Hydration
Drinking large amounts of water to combat rhabdo appears to be a popular home remedy online. While fluid intake may mitigate rhabdo’s damage to the kidneys, it does not address other effects, such as liver and heart issues.
In theory, overhydration could lead to hyponatremia (water intoxication), which can be just as serious as rhabdomyolysis. Some research suggests that hyponatremia may make exercise-induced rhabdomyolysis more likely (Chlíbková et al. 2015).
(Editor’s note: For an in-depth look at hydration, look at Hydration: Through The Lens of Fitness
Rhabdo vs. DOMS
Do not confuse rhabdomyolysis with delayed-onset
muscle soreness (DOMS). While the pain from DOMS and rhabdo may coincide,
there’s an easy way to tell the difference: DOMS hurts only when the exerted
muscles move. It doesn’t hurt when they are at rest.
On the other hand, rhabdo pain is often present at rest—and is frequently described as unbearable. Some people have reported that the pain began soon after they stopped exercising, growing in intensity as the hours went by.
Rhabdo and Pain Relievers
Because people can confuse DOMS with rhabdo, they may be tempted to reach for over-the-counter (OTC) analgesics like aspirin, ibuprofen (Advil) or acetaminophen (Tylenol) to deal with the pain.
As a fitness pro, it’s outside your scope of practice to recommend medications,
but you need to understand that OTC pain relievers can increase stress on the
kidneys and liver, potentially making rhabdo worse. If your clients have
rhabdolike symptoms, refer them immediately to their physician for a formal
diagnosis and proper medical attention.
Rhabdomyolysis Prevention
How can fitness trainers reduce the odds of a client accidently getting rhabdo during workouts?
After reviewing the research and speaking to many who have developed this disorder, I suggest these guidelines:
Novice Training
- Avoid high-volume, high-intensity programs that novices are not accustomed to doing.
- Be careful about single-body-part training or split routines. Spread the exercise stimulus over a wide array of muscle groups.
Circuit Training
- Employ total-body circuit training with lighter resistance. These workouts also improve strength and body composition (Takahata 2018). They are efficient and fit well with the 30-minute personal training sessions typical at many gyms today.
- Because circuit training programs involve more overall movement than multiset programs, they tend to be more fun, especially for beginners. This may translate into greater exercise adherence.
Read also: Circuit Training - Everything You Need to Know
Group Training
Group exercise instructors have a more
difficult challenge because they often do not know who will be in their class
until it begins. To reduce the risk of rhabdo in group classes, adopt these
strategies:

- Take time to educate participants about rhabdo and tell them what to watch out for. Fostering an open environment encourages class attendees to listen to their bodies, work at their own pace and not feel embarrassed if they need to leave class before it’s over.
- Encourage new participants to prepare themselves for a group exercise class by first performing lower-intensity activities on their own, ideally using movements they will experience in the class. For example, suggest they ride a stationary bike on their own for several sessions before taking an indoor group cycling class.
- Offer beginner group exercise classes, which allow people to get familiar with exercises and movement patterns while under the guidance of instructors.
Promote Caution
Exertional rhabdomyolysis sounds scary. And,
yes, it can lead to serious health issues, but it doesn’t have to. Education is
the best defense. Fitness professionals can play a leading role in helping
people understand the risks of rhabdo and know how to grow stronger without
getting hurt.
References
Abbas, M., et al. 2019. A marathon runner
with rhabdomyolysis. Nederlands Tijdschrift voor Geneeskunde, 163, pii:
D2848.
Amezyane, T., et al. 2009. McArdle disease revealed by exercise
intolerance associated with severe rhabdomyolysis. Annals of Endocrinology
(Paris), 70 (6), 480–84.
Atias-Varon, D., et al. 2017. Rhabdomyolysis after crawling military
training. Military Medicine, 182 (7), e1948–52.
Cannon, J. 2017. Can Spinning cause rhabdo? Yes! Here’s the proof.
Accessed Mar. 20, 2019: joe-cannon.com/spinning-rhabdo-review/.
CDC (Centers for Disease Control and Prevention). 1990. Exertional
rhabdomyolysis and acute renal impairment—New York City and Massachusetts,
1988. MMWR Weekly, 39 (42), 751–56.
Chen, C-Y., et al. 2013. Clinical spectrum of rhabdomyolysis presented
to pediatric emergency department. BMC Pediatrics, 13 (134).
Chlíbková, D., et al. 2015. Rhabdomyolysis and exercise-associated
hyponatremia in ultra-bikers and ultra-runners. Journal of the International
Society of Sports Nutrition, 12 (1), 29.
Clarkson, P.M., & Eichner, E.R. 2006. Exertional rhabdomyolysis:
Does elevated blood creatine kinase foretell renal failure? Current Sports
Medicine Reports, 5 (2), 57–60.
Cleary, M.A., et al. 2011. Exertional rhabdomyolysis in an adolescent
athlete during preseason conditioning: A perfect storm. Journal of Strength
and Conditioning Research, 25 (12), 3506–13.
Do, K.D., Bellabarba, C., & Bhananker, S.M. 2007. Exertional
rhabdomyolysis in a bodybuilder following overexertion: A possible link to
creatine overconsumption. Clinical Journal of Sport Medicine, 17 (1),
78–79.
Harrelson, G.L., Fincher, A.L., & Robinson, J.B. 1995. Acute
exertional rhabdomyolysis and its relationship to sickle cell trait. Journal
of Athletic Training, 30 (4), 309–12.
Hein, A. 2018. Police officer who died during training exercise had rare
condition. FoxNews.com. Accessed Mar. 20, 2019: foxnews.com/health/police-officer-who-died-during-training-exercise-had-rare-condition.
Honda, S., et al. 2017. Rhabdomyolysis after high intensity resistance
training. Internal Medicine, 56 (10), 1175–78.
Kao, P.F., et al. 1998. Rectus abdominis rhabdomyolysis after sit ups:
Unexpected detection by bone scan. British Journal of Sports Medicine, 32
(3), 253–54.
Keltz, E., Khan, F.Y., & Mann, G. 2014. Rhabdomyolysis. The role of
diagnostic and prognostic factors. Muscles, Ligaments and Tendons Journal, 3
(4), 303–12.
Kim, J., et al. 2016. Exercise-induced rhabdomyolysis mechanisms and
prevention: A literature review. Journal of Sports Health Science, 5
(3), 324–33.
Knafl, E.G., et al. 2018. Rhabdomyolysis: Patterns, circumstances, and
outcomes of patients presenting to the emergency department. The Ochsner
Journal, 18 (3), 215–21.
Lin, A.C., et al. 2005. Rhabdomyolysis in 119 students after repetitive
exercise. British Journal of Sports Medicine, 39 (1), e3.
Mateo, A. 2018. Amy Purdy: ‘I feared I’d never be able to work out again
after rhabdo.’ Women’s Health. Accessed Mar. 20, 2019:
womenshealthmag.com/fitness/a19643677/amy-purdy-paralympics-rhabdo/.
Nance, J.R., & Mammen, A.L. 2015. Diagnostic evaluation of
rhabdomyolysis. Muscle & Nerve, 51 (6),793–810.
Pattison, M.E., et al. 1988. Exertional heat stroke and acute renal
failure in a young woman. American Journal of Kidney Diseases, 11 (2),
184–87.
Riggs, J.E. 1990. Acute exertional rhabdomyolysis in hypothyroidism: The
result of a reversable defect in glycogenolysis? Military Medicine, 155
(4), 171–72.
Sauret, J.M., Marinides, G., & Wang, G.K. 2002. Rhabdomyolysis. American
Family Physician, 65 (5), 907–13.
Scalco, R.S., et al. 2016. Exertional rhabdomyolysis: Physiological
response or manifestation of an underlying myopathy? BMJ Open Sport &
Exercise Medicine, 2 (1), e000151.
Stanfa, M.R., et al. 2017. Risk factors for collegiate swimmers
hospitalized with exertional rhabdomyolysis. Clinical Journal of Sports
Medicine, 27 (1), 37–45.
Takahata, Y. 2018. Usefulness of circuit training at home for improving
bone mass and muscle mass while losing fat mass in undergraduate female
students. Lipids in Health and Disease, 17 (104).
Thompson, T.L., Nguyen, T.X., & Karodeh, C.R. 2018. Twelve cases of
exertional rhabdomyolysis in college football players from the same institution
over a 23-year span: A descriptive study. The Physician and Sportsmedicine,
46 (3), 331–34.
Tibana, R.A., et al. 2018. Exertional rhabdomyolysis after an extreme
conditioning competition: A case report. Sports, 6 (2), 40.
Tsuruda, T., et al. 2017. Transient left ventricular contractile
dysfunction during the treatment of rhabdomyolysis: A case report and
literature review. Internal Medicine 56 (20), 2797–803.
Vucicevic, Z. 2015. Rhabdomyolysis and acute renal failure after gardening.
Case Reports in Emergency Medicine, 174892.