The COVID-19 virus can have a significant impact on an individual’s health and ability to exercise. The Center for Disease Control (CDC) has noted 11 main COVID-19 symptoms: fever or chills, cough, shortness of breath or difficulty breathing, fatigue, muscle or body aches, headache, the new loss of sensation or smell, sore throat, congestion, or runny nose, nausea or vomiting, and diarrhea (CDC, 2021). Symptoms may appear 2 to 14 days after exposure to the virus and can last up to 6 months in some individuals with long-term complications (Huang et al., 2021).
One of the main hallmark symptoms is respiratory issues such as coughing or shortness of breath (Kakodkar et al., 2020). Experts have begun to look at the positive effects of deep breathing exercises on these respiratory issues among post-COVID-19 individuals (Wang et al., 2020).
This blog discusses the latest research on how the disease affects the respiratory system and using breathing exercises to help clients deal with such complications. You can find more information on managing COVID within the NASM COVID Management Course.
What are the mechanics of breathing (respiration) and primary muscles of breathing and the mechanics ?
The average number of breaths among healthy adults is 12-20 per minute. With inspiration, the rib cage expands through the coordinated contraction of the external intercostals and diaphragm (drops down). The sternocleidomastoid, scalenes, and pectoralis minor also assist with inspiration. With expiration, the rib cage retracts and returns to its resting position
(Table 1). Expiration can be passive with quiet breath. With active expiration, the co-contraction of the internal intercostals and abdominals helps the rib cage retract while the muscles of inspiration relax. This helps forcefully push air out of the lungs as the ribs return to their resting position (Table 2) (Ramirez et al., 2014; Woo et al., 2016).
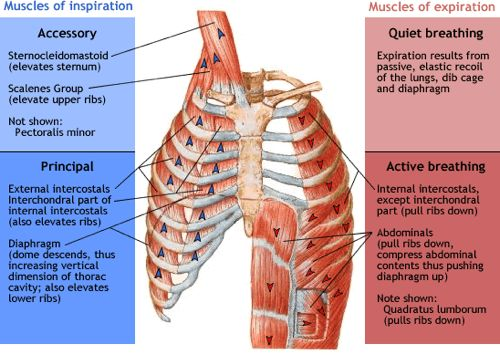
Table 1. Muscle of Inspiration and Expiration.
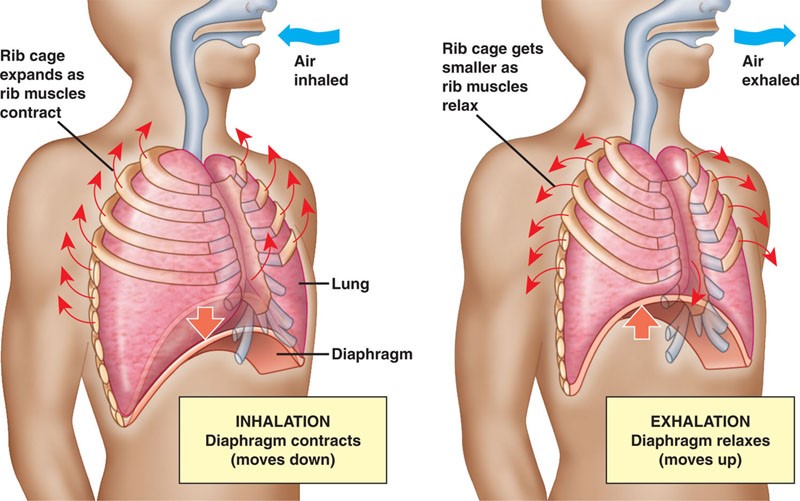
Table 2. Mechanics of Inspiration and Expiration.
Why do some individuals with COVID-19 suffer from respiratory complications?
COVID-19 is the disease process (signs and symptoms) created by the SARS-CoV-2 (severe acute respiratory syndrome coronavirus 2) virus. SARS-CoV-2 is part of the coronavirus family, in which seven variants are known to cause disease in humans (Caldaria et al., 2020). Thus, COVID-19 is a respiratory disease that can infect and cause adverse effects to the lungs (e.g., bronchial tree, alveoli) and other systems of the body (e.g., nervous system).
Experts are still learning about the longer-term effects of the disease among certain people. Individuals with co-morbid medical conditions such as hypertension, heart disease, stroke, and diabetes may suffer from more significant complications (Kakodkar et al., 2020).
Those individuals with severe COVID-19 may be susceptible to pneumonia, acute respiratory distress, fibrosis, and other complications (Torres-Castro et al., 2020). The fitness professional may play a vital role in helping keep these clients healthy, especially if there are suffering from respiratory complications.
What type of respiratory symptoms should a fitness professional look for when training a post-COVID-19 client?
Shortness of breath and fatigue are two common symptoms that post-COVID-19 clients may report. Coughing and chest pain may also be present in some individuals (Lopez-Leon et al., 2021). Respiratory complications can have a profound impact on the client’s ability to exercise. Client’s with difficulties may have a low exercise capacity preventing them from participating in vigorous and/or longer-term cardiorespiratory exercises.
How should post-COVID-19 clients be monitored during exercise?
The fitness professional can monitor clients using blood pressure, heart rate, rate of perceived exertion (RPE), and blood oxygen saturation (Zeng et al., 2020). It is recommended for fitness professionals to take the client’s blood pressure before training and obtain their subjective RPE throughout their exercise program.
The fitness professional can also use a pulse oximeter to monitor their client’s heart rate and blood oxygen saturation (average 95-100%) (CDC, 2021). These monitoring strategies can help ensure a safe exercise session with these clients.
Do breathing exercise help these clients with their respiratory complications?
The short answer is yes! Experts have found that deep breathing exercises positively affect post-COVID-19 individuals with complications (Gloeckl et al., 2021; Wang et al., 2020). The COVID-19 virus is still novel; experts are still studying the effects on the body.
Best practices for the fitness professional should include consulting with the client’s healthcare team (e.g., MD, PT, etc.) before exercise programming to ensure client safety. Fitness professionals need to know that it is safe for a post-COVID-19 client to perform breathing exercises.
COVID Breathing Exercise: DIaphragmatic Breathing
One common breathing technique taught to post-COVID-19 clients is diaphragmatic (sometimes called abdominal) breathing. Diaphragmatic breathing can lower heart rate, blood pressure, reduce stress and anxiety. It may also improve exercise capacity and respiratory function among individuals with pulmonary conditions (Hamasaki, 2020).
This exercise involves lying or sitting while slowly inhaling deep through the nose while slowly exhaling through the mouth with pursed lips. Figure 1 provides some guidelines for diaphragmatic breathing (Wang et al., 2020).
| Diaphragmatic Breathing |
| Lying on your back with knees bent or sitting comfortably. Place one hand on your upper chest and the other on your stomach just below your rib cage. Breathe in slowly through your nose (about 2-3 seconds) so that your stomach will move out against your hand (deep breathe). Slowly exhale through your mouth with pursed lips (as if your blowing out candles or drinking through a straw). Repeat as necessary. | 
|
What are common mindfulness practices that clients can do that involve breathing exercises?
Some mindfulness exercise options for post-COVID-19 clients may include Yoga (e.g., Viniyoga), Pranayama (yoga-related breathing exercises), and Tai Chi. (Wang et al., 2020). All these exercise techniques involve different types of breathing exercises. If clients are not interested in this type of exercise, they can sing a song that also requires coordinated breathing.
This blog provides a brief discussion and the most recent research on breathing exercises for post-COVID-19 clients. The research on the efficacy of deep breathing among these clients is still being studied. Deep breathing exercises are used for a wide variety of conditions. The fitness professional is encouraged to further research breathing exercises and consider them in their client exercise programming.
References:
- Caldaria, A., Conforti, C., Di Meo, N., Dianzani, C., Jafferany, M., Lotti, T., Zalaudek, I., & Giuffrida, R. (2020). COVID-19 and SARS: Differences and similarities. Dermatol Ther, 33(4), e13395-e13395. https://doi.org/10.1111/dth.13395
- CDC. (2021). COVID-19: Symptoms. https://www.cdc.gov/coronavirus/2019-ncov/symptoms-testing/symptoms.html
- Gloeckl, R., Leitl, D., Jarosch, I., Schneeberger, T., Nell, C., Stenzel, N., Vogelmeier, C. F., Kenn, K., & Koczulla, A. R. (2021). Benefits of pulmonary rehabilitation in COVID-19: a prospective observational cohort study. ERJ Open Res, 7(2), 00108-02021. https://doi.org/10.1183/23120541.00108-2021
- Hamasaki, H. (2020). Effects of Diaphragmatic Breathing on Health: A Narrative Review. Medicines (Basel), 7(10), 65. https://doi.org/10.3390/medicines7100065
- Huang, C., Huang, L., Wang, Y., Li, X., Ren, L., Gu, X., Kang, L., Guo, L., Liu, M., Zhou, X., Luo, J., Huang, Z., Tu, S., Zhao, Y., Chen, L., Xu, D., Li, Y., Li, C., Peng, L., Li, Y., Xie, W., Cui, D., Shang, L., Fan, G., Xu, J., Wang, G., Wang, Y., Zhong, J., Wang, C., Wang, J., Zhang, D., & Cao, B. (2021, Jan 16). 6-month consequences of COVID-19 in patients discharged from hospital: a cohort study. Lancet, 397(10270), 220-232. https://doi.org/10.1016/s0140-6736(20)32656-8
- Kakodkar, P., Kaka, N., & Baig, M. N. (2020, Apr 6). A Comprehensive Literature Review on the Clinical Presentation, and Management of the Pandemic Coronavirus Disease 2019 (COVID-19). Cureus, 12(4), e7560. https://doi.org/10.7759/cureus.7560
- Lopez-Leon, S., Wegman-Ostrosky, T., Perelman, C., Sepulveda, R., Rebolledo, P. A., Cuapio, A., & Villapol, S. (2021, Jan 30). More than 50 Long-term effects of COVID-19: a systematic review and meta-analysis. medRxiv. https://doi.org/10.1101/2021.01.27.21250617
- Ramirez, J.-M., Anderson, T. M., & Garcia, A. J., 3rd. (2014). The ins and outs of breathing. Elife, 3, e03375-e03375. https://doi.org/10.7554/eLife.03375
- Torres-Castro, R., Vasconcello-Castillo, L., Alsina-Restoy, X., Solis-Navarro, L., Burgos, F., Puppo, H., & Vilaró, J. (2020, Nov 25). Respiratory function in patients post-infection by COVID-19: a systematic review and meta-analysis. Pulmonology. https://doi.org/10.1016/j.pulmoe.2020.10.013
- Wang, T. J., Chau, B., Lui, M., Lam, G.-T., Lin, N., & Humbert, S. (2020). Physical Medicine and Rehabilitation and Pulmonary Rehabilitation for COVID-19. Am J Phys Med Rehabil, 99(9), 769-774. https://doi.org/10.1097/PHM.0000000000001505
- Woo, S.-D., Kim, T.-H., & Lim, J.-Y. (2016). The effects of breathing with mainly inspiration or expiration on pulmonary function and chest expansion. J Phys Ther Sci, 28(3), 927-931. https://doi.org/10.1589/jpts.28.927
- Zeng, B., Chen, D., Qiu, Z., Zhang, M., Wang, G., Rehabilitation Group of Geriatric Medicine branch of Chinese Medical Association, d. o. M. o. M. R. I. o. C. H. A. R. I. M. d. o. C. R. M. A. d., Wang, J., Yu, P., Wu, X., An, B., Bai, D., Chen, Z., Deng, J., Guo, Q., He, C., Hu, X., Huang, C., Huang, Q., Huang, X., Huang, Z., Li, X., Liang, Z., Liu, G., Liu, P., Ma, C., Ma, H., Mi, Z., Pan, C., Shi, X., Sun, H., Xi, J., Xiao, X., Xu, T., Xu, W., Yang, J., Yang, S., Yang, W., Ye, X., Yun, X., Zhang, A., Zhang, C., Zhang, P., Zhang, Q., Zhao, M., & Zhao, J. (2020). Expert consensus on protocol of rehabilitation for COVID-19 patients using framework and approaches of WHO International Family Classifications. Aging Med (Milton), 3(2), 82-94. https://doi.org/10.1002/agm2.12120