Can a person be fit, yet also be fat? For most of us, a fair assumption would be to believe (at least initially) that the answer is ‘no’, but when you examine the research on this relationship, and the subsequent effects on mortality rates, there is no universal agreement. While plenty of research supports the ‘no’ assumption, a growing number of studies now also support the notion that a person could be fat, yet also be healthy (1, 2). So what are we to believe and use as our compass when it comes to education and programming for activity and weight loss?
First, we should examine definitions of ‘fit’ and ‘fat’ as they alone contribute to this confusion, Then, we should also examine the nature of some of the studies conducted that may have received widespread media coverage without proper merit.
Let’s start first with definitions of overweight and obesity. A measure of body fat percentage would appear to provide a logical assessment of an individual’s level of fat, but the unfortunate reality is that the validity and reliability of in vivo, cost-efficient, field testing for measuring percent body fat remains highly questionable. Consequently, much of science relies upon the more objective measurement of body mass index (BMI) or the Quetelet Index that has replaced the older height-to-weight tables used prior to the mid-1980s.
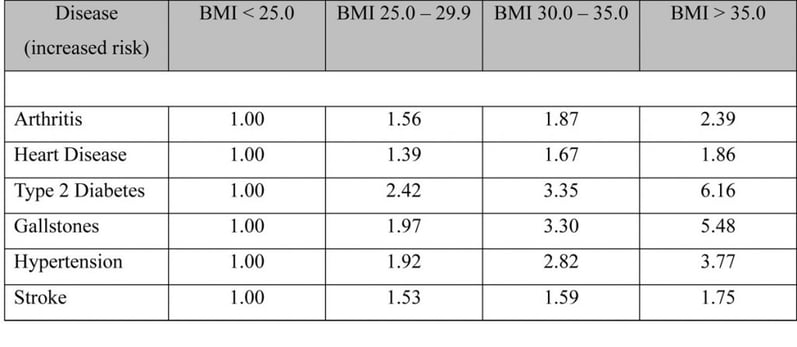
Research supporting mortality to BMI scores (not % fat) is quite strong and defined within the categories established for normal, overweight, obese and morbidly obese (18.5 – 24.9; 25.0 – 29.9; 30.0 – 39.9; 40.0+ respectively) (3, 4). We generally believe that the more body fat a person has, the greater their risk for disease, and because higher BMI scores generally reflect excess fat in most individuals, these scores have been correlated to increased risk of disease (Table 1-1) (3).
Table 1-1: BMI scores and the increased risk for morbidity
Although controversial (as it does not distinguish the source of body weight), one common misconception with BMI is that it is a simple height-to-weight relationship, when in fact it is not. While the calculation uses the measures of height and weight, it is actually a mass-to-surface area relation (Kg/M2) which examines their relationship differently
However, BMI certainly does have limitations with older populations, certain ethnicities (e.g., African-American and Hispanic-American women) and with hypertrophied individuals (to a small degree). To demonstrate this last point and to dispel some mythology around BMI and athletic individuals, consider the following where only one segment of the athletic population skews BMI scores. The standard U.S. formula for calculating BMI = weight (in lbs.) x 703 ÷ height (in inches) ÷ height (in inches):
- Endurance female athlete standing 5’7” and weighing 125 lbs. BMI = 19.57 (normal range)
- Endurance male athlete standing 5’10” and weighing 160 lbs. BMI = 29.96 (normal range)
- Hypertrophied female athlete standing 5’6” and weighing 155 lbs. BMI = 25.01 (cusp of normal to overweight)
- Hypertrophied male athlete standing 5’10” and weighing 220 lbs. BMI = 31.56 (obese category)
Regardless, based upon the information presented, it would appear that individuals with higher BMIs expose themselves to greater risk for morbidity and mortality. But, as mentioned previously, the limitations regarding fit (athletic) individual presents an interesting loophole that researchers have been investigating and it is their discoveries that have provided contradiction to the long-standing notion of fat (i.e., higher BMI scores) and mortality.
One argument stems from the limitation in correlating BMI scores to percentage body fat. For example, a 5’11” male weighing 205 lbs., who is physically active with 12% body fat may be very healthy biometrically, yet measure in with a BMI of 28.6. BMI score of overweight – yes, but according to the National Institutes of Health's (National Heart, Lung and Blood Institute – NHLBI) guidelines on the identification, evaluation and treatment of overweight and obesity in adults, individuals who are overweight can be considered healthy if their waist size is under 35 inches (women) or 40 inches (men), and if they do not have two or more of the following conditions (5):
- Elevated blood pressure
- High blood sugar
- High cholesterol
The NHLBI is not alone in its position – Nichols and colleagues examined data on 43,265 participants enrolled in the Aerobics Center Longitudinal Study between 1979 and 2003 and discovered that overweight and obese people had no greater risk for many diseases and mortality than normal weight people as long as they were metabolically fit despite their excess weight (6).
This term ‘metabolically fit’ describes an individual who may qualify as overweight or obese, yet demonstrates a healthy biometric profile (i.e., no insulin resistance, normal blood sugar levels, healthy lipid profiles and no elevated blood pressure). Interestingly, half of the obese participants in this study qualified as metabolically fit and when comparing their risk of premature mortality against the other obese individuals who had at least two poor health markers, the metabolically fit had a 38% lower risk of premature mortality. It appears that excess weight when combined with metabolic abnormalities is the problem – leading to insulin resistance, hypertension, elevated lipid, etc. Movement and activity involve muscles that utilize blood glucose which maintains insulin sensitivity. Likewise, movement and activity also help regulate blood lipids and blood pressure.
In studies performed by Ekelund and colleagues, and Katzmarzyk and colleagues, they adopted a different approach in examining this concept of metabolic fitness (1, 7). These studies collectively examined the effects of being sedentary plus other lifestyle and biological markers (e.g., obesity) as indicators of mortality. What they both discovered is that movement, or rather the lack thereof, appears to be the leading contributor to pre-mature mortality. Ekelund’s study compared the combined associations between various levels of physical activity, BMI, and waist circumference (WC) with mortality (1).
Physical activity was divided into four categories: inactive, moderately inactive, moderately active and active. Interestingly, the greatest reduction in mortality risk was observed when transitioning between the two lowest activity groups across all levels of general (BMI) and abdominal adiposity (WC). Shifting from being inactive to moderately inactive, regardless of BMI or WC reduced overall mortality rates by 16 – 30%, suggesting that small amounts of movement and activity may be beneficial to improving metabolic health. For example, an average person who stands (e.g., light office activity) for 3½ – 4 hours total a day is considered inactive, but if he or she can manage to include a 20-minute walk each day that expends an additional 100 kcal, that qualifies the person as moderately inactive.
Katzmarzyk’s study by comparison, examined over 17,000 individuals and discovered that sitting, regardless of how much exercise one performed, contributed significantly to premature mortality (7). In other words, the positive effects of exercise and recreational activity appear to be insufficient in undoing all the negative effects of sitting upon metabolic health – sitting increases insulin resistance, elevates triglyceride levels, lowers HDL-cholesterol and decreases lipoprotein lipase (LPL) activity at muscles cells. LPL is the enzyme responsible for fatty acid uptake into muscle cells, which consequently will elevate blood lipid levels and visceral fat deposition when it becomes less active at muscle cells.
Although Kramer and colleagues also supported the notion of metabolic fitness, they did discover that individuals with higher BMI who were metabolically fit still possessed a higher risk of heart disease over comparably metabolically-fit individuals with normal BMI scores (8). Their results did demonstrate however, that it is an unhealthy metabolic state that resulted in a more consistent link to mortality than excess body weight.
But, research also disputes this concept of metabolically-fit. Hogstrom and colleagues examined 1,317,713 younger people who enlisted in the Swedish army between 1969 and 1996 (9). While their findings did correlate an inverse relationship between fitness and mortality in the most fit group (top 20%) and reduced mortality in normal and overweight individuals, it did not do so with obese individuals. Furthermore, they also discovered that unfit normal weight individuals had a 30% reduction in death rates than the more obese, fit individuals. Unlike most studies that examine relationships of mortality with BMI or activity in older population groups, this study investigated outcomes in young men, which may offer some explanation for their findings. This certainly merits further investigation.
Pulsford and colleagues followed 3,720 men and 1,412 women for 16 years, investigating the effects of sitting time (at work, during leisure time, while watching TV, during leisure time excluding TV, and at work and during leisure time combined) as an indicator of mortality (10). Contrary to the findings of Katzmarzyk’s study which demonstrated how sitting behaviors diminish metabolic fitness and subsequently increased all-cause mortality independent of exercise and activity, these researchers found no association.
So, considering the information presented here, what conclusions can we draw? First consider the variants that exist in research design. For instance, in some of these studies the researchers only compared weight with the risk of mortality instead of examining metabolic health – some apparently healthy, but perhaps overweight or obese individuals might have had signs of elevated blood pressure, blood sugar or cholesterol that was not monitored or measured during the study. Although the study by Pulsford and colleagues disputed the existence of metabolic health, a criticism of their study is the fact that while no subjects entered the study with existing or previous heart disease, they never really considered metabolic health throughout their study. Other trials compared healthy, obese or overweight people to unhealthy, obese or overweight people rather than comparing them to normal-weight individuals. Furthermore, many of these studies are longitudinal in design (e.g., longer periods like 16 years) where one can never control or estimate the influence of genetic and environmental variants on study outcomes.
Regardless, one underlying and unifying point appears throughout; although excess fat may increase your risk of morbidity and pre-mature mortality, movement and activity, even in small dosages, coupled with strategies to improve metabolic fitness are our best line of defense for living a long and productive life.
References:
- Ekelund U, et al. (2015). Physical activity and all-cause mortality across levels of overall and abdominal adiposity in European men and women: The European Prospective Investigation into cancer and nutrition study. American Journal of Clinical Nutrition, 2015: doi: 10:3945/ajen.114.100065
- Nichols M, Townsend N, Scarborough P and Rayner M, (2014). Cardiovascular disease in Europe 2014: epidemiological update. European Heat Journal, 35(29): 2950-2959. doi: 10.1093/eurhneart/ehu299
- Berrington de Gonzalez A, et al., (2010). Body-Mass Index and Mortality among 1.46 Million White Adults. New England Journal of Medicine, 363:2211-2219.
- Pan WH, Yeh WT, Chen HJ, Chuang SY, Chang HY, Chen L, and Wahlqvist ML, (2012). The U-shaped relationship between BMI and all-cause mortality contrasts with a progressive increase in medical expenditure: a prospective cohort study. Asia Pacific Journal of Clinical Nutrition, 21(4):577-87.
- Obesity Education Initiative Expert Panel on the Identification, Evaluation, and Treatment of Obesity in Adults (US), (1998). Clinical Guidelines on the Identification, Evaluation, and Treatment of Overweight and Obesity in Adults: The Evidence Report. National Heart, Lung and Blood Institute, Report No.: 98-4083, http://www.ncbi.nlm.nih.gov/books/NBK2003/. Retrieved 01/14/16.
- Nichols M, Townsend N, Scarborough P and Rayner M, (2014). Cardiovascular disease in Europe 2014: epidemiological update. European Heart Journal, 35(29): 2950-2959. doi: 10.1093/eurhneart/ehu299.
- Katzmarzyk PT, Church TS, Craig CL, and Bouchard C, (2009). Sitting time and mortality from all causes, cardiovascular disease and cancer. Medicine and Science in Sports and Exercise, 41(5): 998-1005.
- Kramer CK, Zinman B, and Retnakaran, R (2014). Are Metabolically Healthy Overweight and Obesity Benign Conditions? A Systematic Review and Meta-analysis. Annals of Internal Medicine, 159(11):758-769.
- Hogstrom G, Nordstrom A, and Nordstrom P (2015). Aerobic fitness in late adolescence and the risk of early death: a prospective cohort study of 1.3 million Swedish men. International Journal of Epidemiology, 44(6): December 20, 2015 [epub ahead of print]. doi: 10.1093/ije/dyv321.
- Pulsford RM, Stamatakis E, Britton AR, Brunner EJ and Hillson M (2015). Associations of sitting behaviors with all-cause mortality over a 16-year follow-up: The Whitehall II study. International Journal of Epidemiology, 44(6): 1909-1916.