Proper assessment and training of the foot musculature are vital to optimal health . Given that the feet are our foundation and interact with our environment daily, it affects the whole body if they hurt. The American Orthopaedic Foot and Ankle Society categorizes problematic foot and ankle issues by specific area: Ankle, midfoot, heel and big toe are primary categories (AOFAS 2019).
However, given the abundance of research, data and overall information on foot and ankle conditions, there is not enough room to cover every category here, so this article will take a narrower focus: the midfoot and the heel.
The Foot Bone’s Connected to the . . .
As the old song goes, “The foot bone’s connected to the . . . hip
bone”? At some point in their education, fitness professionals learn about the kinetic chain.
This has been described as “the interconnected linkage of all joints in the body,” which allows force to be transferred from the nervous system to the muscular and skeletal systems (NASM 2014). In other words, movement of the foot influences the knee, the hip and even the spine. Here is a review of these influences, working from the ankle upward.
Subtalar joint to tibia
Motion at the subtalar joint has a direct link to motion in the tibia. As the subtalar joint pronates, the tibia internally rotates, and as the subtalar joint supinates, the tibia goes into external rotation (Powers 2003). The reverse is also true: The subtalar joint responds as movement is induced in the tibia.
Tibia to femur
It is important to recognize that during functional tasks, such as walking, running, squatting and so on, the femur responds to movement of the tibia. During internal tibial rotation, the femur moves into internal rotation and adduction. Conversely, during external tibial rotation, the femur moves into external rotation and abduction (Powers 2003).
Femur to pelvis
As the femur moves, so must the pelvis. An excellent example of this pelvic motion comes from a study conducted by Khamis et al. (2015), who found that inducing hyperpronation with a lateral wedge significantly affected lower-extremity and pelvic alignment.
The researchers concluded that foot pronation caused internal rotation of the
tibia, further leading to internal femoral rotation and a subsequent anterior
tilting of the pelvis (i.e., the front of the pelvis moved toward the floor).
In an earlier study, Rothbart and Estabrook (1988) indicated that excessive
pronation during gait leads to a functional shortening of the leg and an
anterior pelvic tilt, which may eventually cause weakness of the glutes and
sacroiliac joint dysfunction.
Functional changes in the foot can also impair optimal muscle-firing sequences at the hip. Lee, Jeong & Freivalds (2001) demonstrated that a 2- and 3-inch heel lift induced a 45- and 60-degree anterior pelvic tilt, respectively. Further, Mika, Clark
& Oleksy (2013) found that a heel lift of more than 3.5 inches (10 centimeters) led to significantly earlier contraction of the erector spinae and delayed firing of the gluteus maximus during trunk flexion tasks.
Granted, 10 cm is higher than the average high-heeled shoe. However, it should be clear that changes in the foot’s position significantly affect function in the rest
of the body.
Core to subtalar joint
While the importance of a solid foundation cannot be overstated, one must also be cognizant of foot dysfunction that originates at the core. In a thorough review of the literature, Barton et al. (2013) concluded that delayed firing of the gluteus
medius or reduced endurance in this muscle was associated with poor hip control
in the frontal and transverse planes. A lack of control at the hip is likely to
allow internal femoral rotation and alter kinematics at the knee.
As discussed in the previous paragraphs, if movement of the subtalar joint causes movement in the tibia, which in turn causes movement in the femur, then it is reasonable to assume that the effects can trickle downward, too: Movement in the femur can cause movement in the tibia, which can then cause movement at the subtalar joint (i.e., foot flattening or excessive pronation).
Foot to . . . anything else?
Fitness professionals must recognize that foot dysfunction is never isolated to the foot. Other dysfunctions, such as knee, lower-back or even neck issues, may be related to the foot and ankle. Or, perhaps, foot dysfunction itself is originating from somewhere up the chain. Therefore, if fit pros are going to provide the best program possible, both the assessment process and the ideal intervention need to isolate and address the many potential causes of a problem.
The Midfoot: Low Arches
The midfoot—the area just in front of the heel and behind the
metatarsal joints—is a key site of foot pain. A low arch or flat foot is one of
the most common conditions of the midfoot.
All too often, individuals with flat feet choose to mask the problem by purchasing a simple over-the-counter insole versus truly taking the time to identify the root cause of the problem and come up with a probable solution.
Flat Feet: Causes and characteristics

Flat feet can be caused by a deformity in the bony structure of the foot (i.e., the bones do not form an arch naturally), or the cause may be functional (i.e., there is an arch, but the muscles have become too weak to maintain it). A flat foot has been defined as “medial rotation and plantar flexion of the talus, eversion of the
calcaneus, collapsed medial arch and abduction of the forefoot” (Pita-Fernandez
et al. 2017). Thus, it is clear that a flat foot is a multidimensional impairment. This should provide insight into the difficulty in diagnosing and
treating the condition.
Pita-Fernandez et al. found that more than 26% of a random population sample (n = 835) demonstrated clinically flat feet. These individuals were, on average, older (about age 65) and had a higher body mass index (~31.5). Interestingly, the authors stated that flat feet were not just painful in many participants; they also led to lower quality of life as compared with normal foot arches.
Treatments
Common approaches for treating painful flat feet are the use of orthotics (arch-supporting shoe inserts) and participation in physical therapy, depending on the etiology of the condition. However, unless the issue is caused by a structural deformity of the bones, using inserts is simply masking the problem.
While this may prove advantageous in the short term, relying too heavily on orthotics may lead to other problems in the long term, such as altered knee and hip mechanics.
Heel Pain and Plantar Fasciitis
Heel pain has often been described and categorized as plantar
fasciitis, stone bruise or a heel spur (AOFAS 2019). In reality, most people
tend to self-diagnose all heel pain as plantar fasciitis.
However, this diagnosis can sometimes be false because, while the plantar fascia may indeed be irritated, it could be degeneration of tissue or irritation of nerves near the heel that is causing the problem.
For that reason, this article will focus on the general meaning of plantar fasciitis (i.e., irritation of the plantar fascia).
Causes and characteristics
Muth (2017) defined plantar fasciitis simply as irritation or straining of the plantar fascia, a band of tissue that runs along the bottom of the foot. The most common symptoms are pain near the heel or pain in the arch of the foot.
The causes of plantar fasciitis can vary from excess weight to excess activity to excessively pronated or excessively supinated feet. Among exercisers, the condition is more often found in people who perform high-impact activities like running, jumping or dancing.
However, the important thing to remember is that, regardless of the root cause, it is excessive strain on the tissue that leads to pain and discomfort.
Treatments
Gutteck, Schilde & Delank (2019) more eloquently explained plantar fasciitis as “multifactorial in origin and . . . a mechanical overloading reaction to multiple
instances of microtrauma.” One potential cause of excess loading of the plantar
fascia is decreased range of motion in the posterior lower leg.
Patel & DiGiovanni (2011) found that out of 254 patients, 211 had limited ankle
dorsiflexion, 154 had restriction in the gastrocnemius, and 66 had restriction
in both the gastrocnemius and soleus.
These are key findings, since they indicate that identifying and improving ankle dorsiflexion may be the first step in reducing repetitive mechanical loading of the plantar fascia.
Assessments: Where Does the Problem Start?
The foot is one of the most complex areas of the body, considering
how many bones, joints and muscles the foot has and how many complex movements it can perform. Bowman (2017) explains that each bone in the foot—there are 26—is capable of individual movement in multiple planes. Thus, calculating the total number of movements takes a rather high-tech calculator.
For this reason, the assessments discussed here are more global and are intended to help the corrective exercise specialist or personal trainer to identify those compensatory movements that are the most closely related to kinetic-chain dysfunction or injury.
Following the sequence allows you to rule out various problems—and hone
in on where the compensation is originating.
Note: It is very important for any person experiencing pain in the foot (or elsewhere) to have a full, thorough assessment completed by a physician.
Overhead Squat Assessment
During the OHSA, a client should be able to (1) keep the feet pointing straight ahead with knees in line with the second and third toes; (2) keep close-to-neutral alignment in the ankle and subtalar joint (some flattening of the foot is expected during the descent into a squat); and (3) maintain parallel lines between the torso and tibia.

Deviations at these checkpoints may include the feet flattening and turning out, the knees moving inward, or the torso leaning forward excessively.
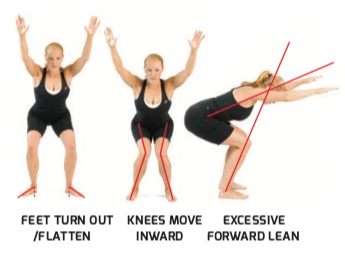
The most common set of compensations is the foot flattening and turning out, along with associated knee valgus, a combination otherwise known as pronation distortion syndrome (PDS).
PDS is the exact culmination of events discussed earlier in the article, as the condition is the result of compensatory movement in the subtalar joint, obligatory internal rotation of the tibia, and internal rotation and adduction of the femur. As noted, this often leads to movement in the pelvis and additional biomechanical problems, as well.
PDS compensations are closely associated with the common aches and pains of the foot. The flattening and turning out of the foot can overload the plantar fascia, causing midfoot or heel pain.
If a client demonstrates PDS or any of the compensations outlined
in the preceding paragraph, the next step is to attempt to isolate where the
problem is stemming from—ankle or hip.
Heels-Elevated Squat Assessment
Squatting with the heels elevated takes the calf muscles and ankle
joint out of the equation by placing the ankle in plantar flexion. If the
compensations disappear during this version of the squat, then the root cause
of the compensation (whether it is excessive flattening of the foot or
excessive forward leaning) is the foot and ankle complex.
When the calves are short and limit optimal dorsiflexion, it is very common during a squat for the feet to flatten or turn out or for the person to lean far forward. Thus, by removing the tight muscle from the equation, the compensations usually clear up.

It is important to recognize that elevating the heels is used only during the assessment and should not be the correction for this condition. Instead, a program focusing on the foot and ankle should be developed and implemented.
However, if the compensation remains, then the problem is originating somewhere farther up the kinetic chain, most likely in the hips or pelvis.
Single-Leg Squat Assessment
If a client did not compensate during the two-legged squat, a
single-leg squat is then recommended. The increased stabilization that this
move demands will often expose underlying compensations.

The ones to look for during a single-leg squat are the foot flattening and the knee moving inward (left). If one or both of these compensations are noted, the individual may perform the single-leg squat with heel elevated, but only if there is enough foundational balance to complete the move safely, as this is like squatting in a high-heeled shoe.
If the modification corrects the compensation, then the cause of the compensation is at the foot and ankle. If the modification does not correct the compensation, then the sample program for the hip (below) may be helpful.
Help Clients Put Their Best Foot Forward
In conclusion, although the foot is a complex area of the body, following a simple assessment logic can help identify the root causes of compensations that could lead to aches, pains and other dysfunctions if not addressed. In reviewing this article, fitness professionals should begin to recognize the many compensatory patterns that can stem from or cause foot and ankle dysfunction. With this information, fit pros can create a program or programs designed to address those compensations and, hopefully, prevent future pain—from the ground up!
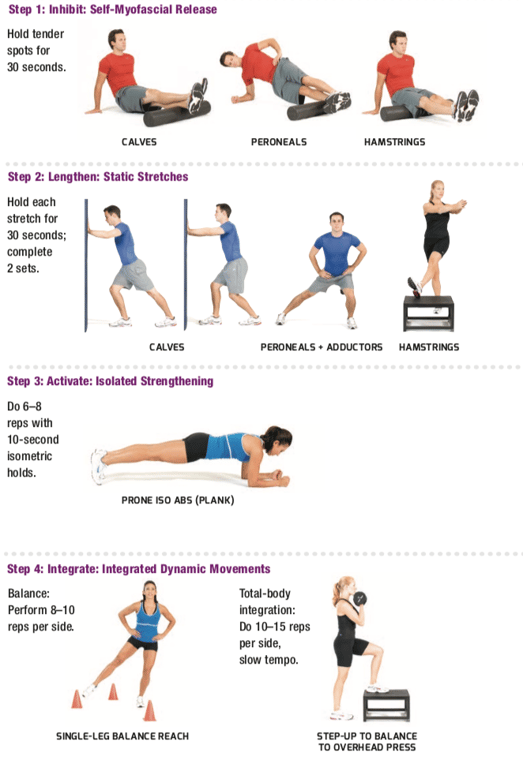
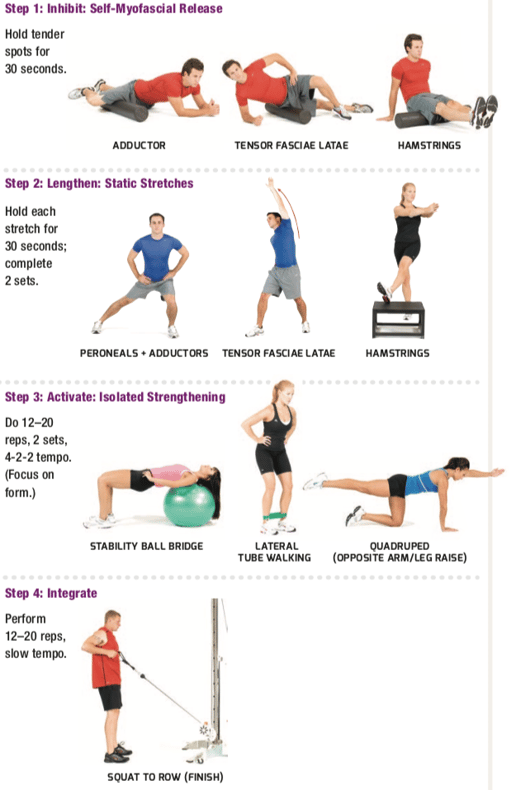
Sample: Two Integrated Programs
Both sample programs shown here can be a part
of a client’s weekly training sessions. Which program is primary and receives
most attention will depend on the problem’s root cause: foot and ankle or hip
and pelvis. For example, if the foot and ankle are chief concerns, the client
might perform the Foot and Ankle Stabilization Endurance Program 3–4 days per
week while completing the Hip Stabilization Endurance Program only 2–3 days per
week.
Foot and Ankle Stabilization Endurance Program
If the foot and ankle are identified as the root cause, then a stabilization endurance program specific to the foot should be implemented. The program begins with foam rolling and static stretching of overactive muscles such as the gastrocnemius/soleus (calves), peroneals and biceps femoris (hamstrings).
Then comes a basic core exercise, such as a prone or side plank, to wake up the important stabilizers. The next step integrates balance training, which fires underactive muscles such as the intrinsic muscles of the foot, including the posterior and anterior tibialis.
The program then concludes with a total-body integration exercise.
Hip Stabilization Endurance Program
If the foot and ankle are not identified as the root cause, then a simple hip program should be implemented.
The program begins with foam rolling and static stretching of the adductors, tensor fasciae latae and biceps femoris.
The next step is core activation, which should focus on the gluteus maximus/medius and core stabilizers.
The program then concludes with a total-body integration exercise.
Interested in corrective exercise? Find out how you can benefit from the NASM Corrective Exercise Specialization.
References
AOFAS
(American Orthopaedic Foot & Ankle Society). 2019. Conditions. Accessed
Apr. 14, 2019: legacy.aofas.org/footcaremd/conditions/Pages/conditions.aspx.
Barton,
C.J., et al. 2012. Gluteal muscle activity and patellofemoral pain syndrome: A
systematic review. British
Journal of Sports Medicine, 47 (4), 207–14.
Bowman,
K. 2017. Move Your DNA:
Restore Your Health Through Natural Movement: Expanded Edition
(2nd ed.). Sequim, WA: Propriometrics Press.
Gutteck,
N., Schilde, S., & Delank, K.S. 2019. Pain on the plantar surface of the
foot. Deutsches Ärzteblatt
International, 116 (6), 83–88.
Khamis,
S., et al. 2015. The relationship between foot and pelvic alignment while
standing. Journal of Human
Kinetics, 46, 85–97.
Lee,
C-M., Jeong, E-H., & Freivalds, A. 2001. Biomechanical effects of wearing
high-heeled shoes. International
Journal of Industrial Ergonomics, 28 (6), 321–26.
Mika,
A., Clark, B.C., & Oleksy, L. 2013. The influence of high and low heeled
shoes on EMG timing characteristics of the lumbar and hip extensor complex
during trunk forward flexion and return task. Manual
Therapy, 18 (6), 506–11.
Muth,
C.C. 2017. Plantar fasciitis. JAMA,
318 (4), 400.
NASM
(National Academy of Sports Medicine.) 2014. NASM
Essentials of Corrective Exercise Training (1st rev. ed.).
Burlington, MA: Jones & Bartlett Learning.
Patel,
A., & DiGiovanni, B. 2011. Association between plantar fasciitis and
isolated contracture of the gastrocnemius. Foot
& Ankle International: SAGE Journals, 32 (1), 5–8.
Pita-Fernandez,
S., et al. 2017. Flat foot in a random population and its impact on quality of
life and functionality. Journal of
Clinical & Diagnostic Research, 11 (4), LC22–27.
Powers,
C.M. 2003. The influence of altered lower-extremity kinematics on patellofemoral
joint dysfunction: A theoretical perspective. Journal
of Orthopaedic & Sports Physical Therapy, 33 (11), 639–46.
Rothbart,
B.A., & Estabrook, L. 1988. Excessive pronation: A major biomechanical
determinant in the development of chondromalacia and pelvic lists. Journal of Manipulative &
Physiological Therapeutics, 11 (5), 373–79.
















