The average American consumes 3,436 mg of sodium each day, an amount far in excess of the tolerable upper level (UL*) intake recommended by most health organizations to prevent health concerns like hypertension, a disease attributed to nearly 400,000 deaths each year (1-2).
Almost 200,000 of these deaths occur in women, which, by comparison is five times higher than the annual death rate from cancer in women. Although this UL is set at 2,300 mg a day, the American Heart Association (AHA) and Institutes of Medicine (IOM) recommend a lower daily intake of 1,500 mg to promote good health, especially in older adults and in individuals exhibiting increased risks for heart disease (2-4).
Sidebar: A UL refers to the highest daily level of a compound that is likely not to pose an adverse health risk or effect to almost all individuals in the general population.
To help gain a more practical perspective of what these amounts mean, consider first that common table salt or sodium chloride (our greatest source of dietary sodium) contains approximately 40 percent sodium by weight. Therefore, a full teaspoon of salt weighing 5,750 mg contains approximately 2,300 mg of sodium, the equivalent of the UL suggested for adults, whereas a little more than a ½ teaspoon of salt provides the recommended 1,500 mg of sodium.
Learn more about daily sodium levels and other micronutrients here.
Hypertension concerns
The obvious concern with excessive sodium intake involves hypertension given the dose-related relationship that exists between sodium intake and high blood pressure (4). High blood pressure is considered a major risk factor in heart disease and stroke, our first and third leading causes of death, respectively (4). Because sodium increases water retention, larger intakes increase blood volume, which in turn increases the pressure exerted on the arteries.
To learn about a diet specifically catered to lower blood pressure, check out our DASH Diet guide.
When salt intake is reduced, systolic blood pressure (SBP) can be lowered by 2 – 8 mm Hg within a few days to a few weeks. In addition to reducing salt intake, other lifestyle-related factors can also positively influence blood pressure scores (4-5). For example, losing weight can reduce resting SBP by 5 – 20 mm Hg; physical activity can reduce SBP by 4 – 9 mm Hg, while reduced alcohol intake can also lower SBP by 2 – 4 mm Hg.
But, sodium doesn’t just affect your health, as it can impact your physical appearance as well. Excessive intakes of sodium can increase symptoms and feelings of puffiness, bloating, and lead to weight gain.
The human body needs between 180 and 500 mg of sodium per day to complete various physiological functions that include (1):
- Maintaining fluid volume (in blood) and blood pressure.
- Maintaining fluid balance and osmotic pressure between our two primary water compartments of the body (intracellular and extracellular fluid).
- Enabling nerve conduction and muscle contraction.
- Formation of gastric acid in the stomach to assist with digestion, digestive enzyme activation, and to fight foreign bodies.
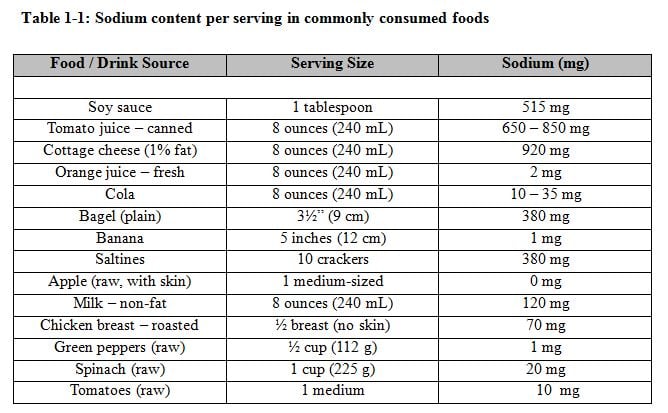
- Formation of our lactate buffer (sodium bicarbonate), a critical buffer needed during high-intensity exercise.
The vast majority of our dietary sodium is found in processed retail and restaurant foods – 65% originating from retail foods; 25 – 30% from restaurants, and 20 – 25% from food cooked at home or from salt used at the at table (1). Many foods contain sodium (nuts, dill pickles, olives, salsas, etc.,), but the most common sodium-containing foods include pizza, many commercially-prepared entrees, bread and rolls, cold and cured meats, poultry, sandwiches and soups, with some canned soups containing as much as 1,000 milligrams of sodium per serving (Table 1-1).
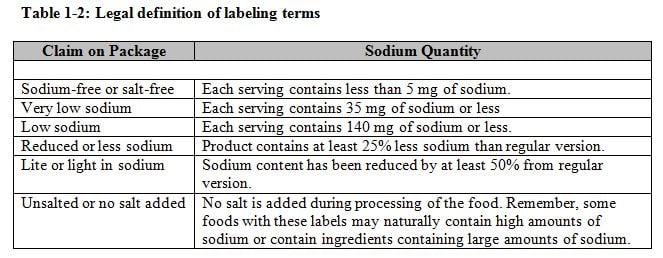
 Reading sodium content on nutritional labels is an effective strategy for building awareness and making healthier choices. But, labels can also be confusing regarding the claims made regarding the sodium quantity in a product. It may therefore prove helpful to understand the legal definitions of labeling terminology used by manufacturers on their products (Table 1-2).
Reading sodium content on nutritional labels is an effective strategy for building awareness and making healthier choices. But, labels can also be confusing regarding the claims made regarding the sodium quantity in a product. It may therefore prove helpful to understand the legal definitions of labeling terminology used by manufacturers on their products (Table 1-2).
The benefits of sea salt
Sea salt is considered by some to be a natural and healthy salt alternative – made from evaporated seawater that undergoes minimal processing unlike table salt that produces salt’s fine texture. Its popularity has boomed, but unfortunately, it contains almost equal quantities of sodium as processed table salt.
Almost all individuals can benefit from reducing their sodium intake that can be achieved via some simple dietary strategies (6):
- Select more fresh foods like fruits and vegetables as they are naturally low in sodium.
- Fresh cuts of meat and poultry minus the sodium-containing solutions often injected into these products contain less sodium than cured luncheon meat, bacon, hot dogs, sausage, and ham.
- Select plain whole-grain rice and pasta products over products containing added seasonings.
- Remove salt from recipes whenever possible (season with herbs, spices and other flavorings).
- Limit the use of sodium-rich condiments like soy sauce, salad dressings, dips, ketchup, mustard, and relish.
- Avoid foods containing more than 200 mg of sodium per serving and also consider how many servings you plan to consume.
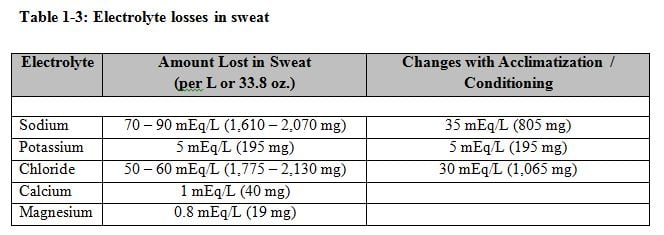
In the realm of exercise, sweat, electrolyte losses and possible hyponatremia all merit consideration. Sodium is the most important electrolyte lost during sweating because it exists primarily in the extracellular fluid compartments, the region from where most sweat losses originate (3). The information provided in Table 1-3 illustrates why beverages consumed during exercise or sweating should favor sodium over a potassium-rich beverage like coconut water.
Read also: Foods to Restore Electrolytes
Sodium not only enhances the palatability of sports drinks, but it also replaces sodium loss associated with sweating. This is needed to help preserve or replace total body water and can prevent hyponatremia, a potentially fatal condition characterized by lowered plasma sodium level (< 135 mmol/L). By only replacing water (blood-dilution effect) during or after sweating, this dilution effect allows more water to cross into the brain cells, potentially triggering brain tissue swelling (i.e. cerebral edema).
Initial symptoms include fatigue and confusion, but it can then lead to more serious conditions such as seizures, and even coma and death. Although this condition is rare, affecting 0.6% of the marathon population and almost 0% of the general population, it can be avoided by consuming some sodium during exercise. While sweat rates vary between individuals, the sodium replacement recommendation provided by the IOM for sweating range between 72 and 168 mg per every 8 oz. serving of fluid (3).
One primary effort for improving cardiovascular health involves a reduction in our dietary intake of sodium to a target of 1,500 mg a day. From an economic perspective, reducing the sodium intake of Americans by 1,200 mg per day on average can save up to $20 billion a year in medical costs (1). As salt is often used to flavor foods and believed to be an acquired taste, it is possible that individuals can gradually decrease their overall sodium intake towards ¼ teaspoon daily and learn to enjoy less as taste buds adjust.
Sodium intake can enhance sports performance, but so can Iron as well! Check out this blog to continue learning about crucial micronutrients for sports performance.
References:
- Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion (2009). Sodium Fact Sheet, www.cdc.gov (retrieved June, 2014).
- U.S. Department of Health and Human Services, U.S. Department of Agriculture. (2010). Dietary Guidelines for Americans. Washington, DC: Government Publishing Office.
- Institute of Medicine, (2005). Dietary reference intakes for water, potassium, sodium chloride, and sulfate (1st edition). Washington, DC: The National Academies Press.
- American Heart Association, (2012). Sodium Recommendations.www.aha.org (retrieved June, 2014).
- Public Health Services, National Institutes of Health, National Heart Lung and Blood Institute, (2003). Seventh Report of the Joint Committee on Detection, Evaluation, and Treatment of High Blood Pressure (JNC VI). NIH Publication, No. 03-5233.
- Institute of Medicine (2010) Strategies to Reduce Sodium Intake in the United States. Washington, DC: The National Academies Press.