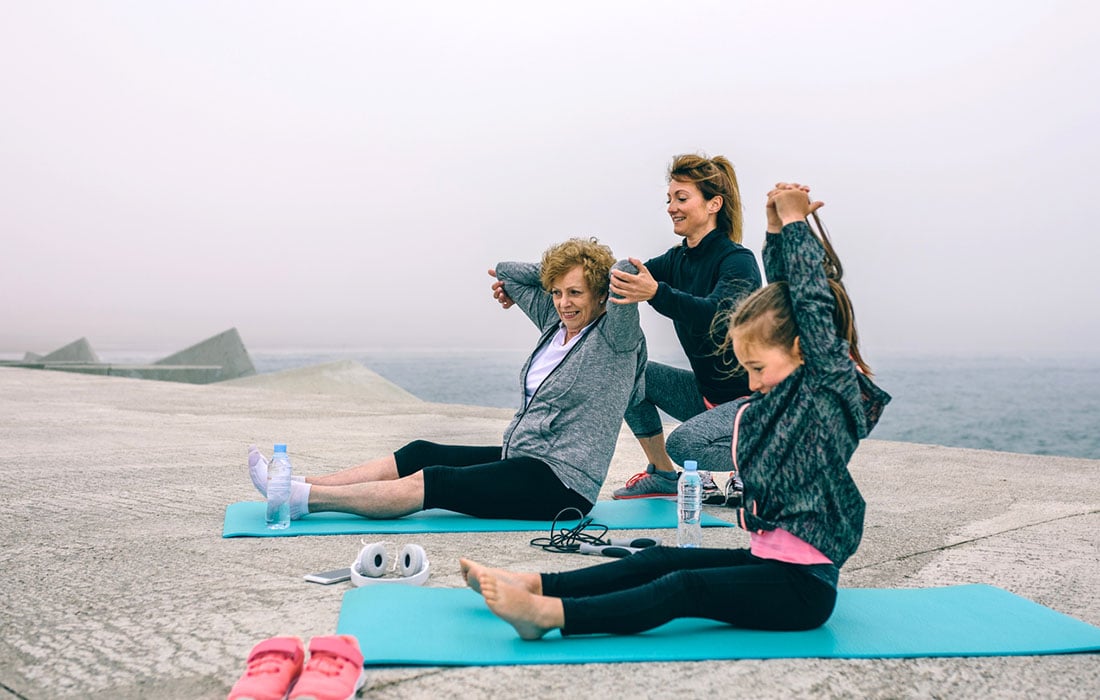
A skilled fitness professional should have the capacity to handle a variety of special populations. The needs and training goals of older adults and children differ greatly from those of teens or young and middle adults. Generally, the most common reason for a young or middle- aged adult to hire a personal trainer is weight loss (Melton et al., 2008), however, that goal is not always appropriate for older adults or youth.
This training guide examines the most common training goals of these populations and provides the fitness professional with guidance for assessment and programming. If you are a Youth Exercise or Senior Fitness Specialist.
Follow each jump link to navigate to each section of this training guide for special populations:
To learn about training for older adults:
- Training Benefits
- Appropriate Exercises
- Fitness Assessments
- Overhead Squat
- Balance
- Cardio
- Muscle-Strength
- Program Design
To learn about training for children:
- Benefits of Training Youth
- Physiologic Considerations
- S.M.A.R.T Training Goals
- Movement Assessments for Children
- Program Designs
- Keeping it Fun for Kids
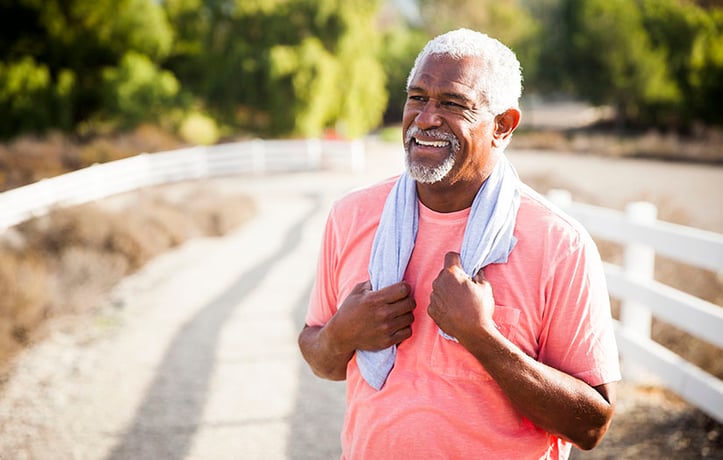
training benefits for older adults
Regular exercise and training in older adults can improve flexibility, improve balance and coordination, decrease the risk of falls, enhance glucose tolerance and insulin sensitivity, improve reaction time and can help maintain healthy blood lipid values (Powers & Howley, 2018). Most importantly, regular training can assist an older adult in maintaining independence (Shephard, 1993).
Exercise can promote and prolong independence in older adults. Oftentimes, functional goals are more appropriate for these clients than significant weight loss. In fact, weight loss goals for older adults can sometimes be dangerous for their overall health.
Approximately 25% of weight loss attempted by older adults intentionally can result in a significant decrease in muscle mass. Weight loss in older females carries a 1.8 times greater risk of hip fracture.
Although high BMI can also be a health hazard, it is more appropriate to direct older clients to exercise regularly, set reasonable goals and consume a nutrient dense moderate diet to promote overall health (Gill et al., 2015).
how to determine Appropriate exercises for older populations
The current recommendations for exercise prescription in older adults indicate that the exercise program should include 150-300 minutes per week of moderate aerobic activity (or 75- 150 minutes of vigorous aerobic activity), a flexibility and balance component at least twice weekly and strength (resistance) training at least twice weekly (Ann Yelmokas McDermott & Mernitz, 2013).
Completing assessments in conjunction with appropriate exercise prescription guidelines can help the trainer and client develop SMART (specific, measurable, attainable, realistic and timely) goals together.
Goals related to strength gains, increases in lean body mass, increases in VO2 max, ease of performing activities of daily living (ADLs), improvement in lipid levels and insulin sensitivity and exercise compliance are appropriate for this population (Clark et al., 2014).
For more on exercise selection for older populations, watch this video on training Seniors with the OPT Model
fitness assesment basics for older adults
Assessments drive training programs for all individuals. There are several assessments that are recommended specifically for older adults. It is critical that the potential client complete a Physical Activity Readiness Questionnaire (PAR-Q).
This population of clients is more prone to special conditions such as diabetes, hypertension, dyslipidemia, cancer, coronary artery disease, osteoporosis, severe muscle atrophy and other orthopedic issues.
A careful medical history including medication usage should help the fitness professional screen for these special conditions. Please note that these conditions carry their own set of recommendations for training programs.
Postural assessment can help the trainer identify abnormalities such as forward head position, lordosis or kyphosis. Forward head posture can be associated with respiratory distress and individuals with kyphosis can have difficulty with ADLs and have an increased risk of falls, vertebral fractures and premature death. Likewise, postural deviations can indicate the presence of other disease processes such as osteoporosis, proprioceptive deficits, and muscle degradation (Roghani et al., 2017).
Overhead Squat Assessments for older populations
Overhead squat assessments (OHSA) are recommended to screen for baseline movement dysfunction. However, many older adults may not be comfortable squatting or may not have the ability to complete the test. Instructing the client to assume the overheat squat assessment positioning (toes pointed forward, arms straight up overhead) while proceeding to sit in a chair is a reasonable modification for these clients.
Oftentimes, without the modification, the OHSA may yield false results (such as an inadequate forward lean) as the client may not be able to attain low enough squat depth to adequately screen for movement dysfunction (Brookbush, 2017). The OHSA can detect specific flexibility limitations based on the movement compensations identified (Clark et al., 2014).
Likewise, it is important to refer to the PAR-Q form and medical history to make certain that the client does not have movement limitations significant enough to contraindicate the OHSA. Single leg squat assessments should be avoided in some clients (especially with balance
difficulties because of the risk of falls, however, in some older adults, the ability to perform a single leg squat predicts the ability to navigate stairs. The fitness professional should make a cautious determination as to whether the single leg squat assessment is warranted or safe (Hockings et al., 2013).
how to do balance assessments for older adults
Balance assessments are also recommended when working with older adults as this is an area where there are often deficits. The gold standard assessment for balance in older adults is the Berg Balance Scale which is also used in clinical settings. The BBS assessment requires the participant to perform several balance related tasks under the supervision of a fitness professional, physical therapist or physical therapy assistant who will then score the assessment.
A score of 0-20 indicates a high fall risk, a score of 21-40 indicates a medium fall risk and a score of 41-56 indicates a low fall risk. Note that clients that are a high fall risk, especially if they have co-morbidities, may warrant referral to a physical therapist (Sanders, 2014).
cardio considerations and the rockport walk test
Cardio-respiratory efficiency can be measured via VO2 max assessment. Although a YMCA 3- minute step test is a quick and easy assessment that requires little equipment, many clients in this population may have pre-existing joint problems which would contraindicate the use of a 12-inch step. The 6-minute walk test is a reliable alternative in this population that can provide baseline information on functional and cardio-respiratory status (Enright et al., 2003).
The Rockport Walk test can also be safe alternative VO2 max assessment in older adults and requires less equipment to complete (Fenstermaker et al., 1992). Cardio-respiratory assessments should be repeated periodically to track the client’s progress towards improving VO2 max and overall cardio-respiratory efficiency.
Muscle-Strength assessments for older populations
Muscle strength assessments can also be a useful tool in determining weight selection for an older adult’s training program. Two tests that are easy to perform in the fitness facility setting are the Chair Stand Test and the Arm Curl Test. The Chair Stand test requires the client to stand up from a seated position without using their arms and return to a seated position.
The goal of the test is to complete as many repetitions as possible in a 30 second time frame. If the client is unable to perform at least 8 full repetitions, they may be at risk for functional limitation. The second test requires the participant to complete as many repetitions of a standard bicep curl as they can complete in a 30 second time period. It is advisable to test both arms to determine if the client has asymmetry.
These assessments can be completed periodically as the client progresses through a training program (Rikli & Jones, 2013)
Other assessments may be necessary depending on the client’s history and reports of pain or range of motion limitation. Additional upper extremity assessments such as an abduction test, rotation test, shoulder flexion test may be warranted if range of motion limitations are suspected or the OHSA reveals a compensation pattern such as the arms falling forward (Clark et al., 2014).
facets of program design to keep in mind
The results of the assessments will drive the development of the training program. For instance, a client who has an exceptionally low VO2 max score will start with lower intensity aerobic exercise and build slowly towards more moderate intensity activity. Likewise, a client who has poor balance may require additional balance training and regressions with their strength training (such as using more stable surfaces, performing exercises in seated positions, etc).
Aerobic exercise should be prescribed at the recommended frequencies unless not tolerated by the client.The recommendations for strength training program prescriptions in older adults indicate that strength training should be performed twice weekly with two sets of 8-12 repetitions being performed in all major muscle groups.
The results of the OHSA can help the fitness professional determine an overall training plan that includes flexibility, balance and strength training for the client by applying the Optimum Performance Training Model (OPT Model).
Training programs should begin the Stabilization Endurance phase (if more specific corrective exercises are not needed) and progress to the Strength Endurance phase. Continuous periodization of these two phases can adequately meet most balance, flexibility and strength training needs of older adults (Clark et al., 2014).
It is important to remember that training plans must be designed specifically for the individual client. The fitness professional must refer to training guidelines for specific conditions and co-morbidities and special needs when designing programs for older adults.
Benefits of training Youth and Children
Children under the age of 13 years old can benefit greatly from regular exercise (both aerobic and strength training). The Centers for Disease Control (2020) recommends that children engage in 60 minutes of moderate to vigorous exercise daily. This should include flexibility, balance, strength and aerobic training.
Regular exercise also promotes enhanced neuromuscular control, increased bone mass, enhanced academic scores and improvement in overall self-esteem and self-efficacy (Centers for Disease Control, 2020). Typically, goal directed training should begin around the age of 7-8 when the individual has developed appropriate maturity and proprioception (Dahab & McCambridge, 2009).
Kamijo et al. (2011) conducted a 9-month randomized controlled trial to examine the effects of regular aerobic activity on cognition in school aged children. The results indicated that the participants performed better as compared to the control group on working memory tasks (Kamijo et al., 2011). Lazaar et al. (2007) demonstrated that increased physical activity significantly improved body composition in obese children over a 6-month period (Lazaar et al., 2007).
Physiologic Considerations for training children
Children are not small adults. There are differences in physiologic adaptations to exercise in children under the age of 13 that differ from adults. First, children have undeveloped sweat glands and often attain a higher core temperature during exercise than adults.
Children need more blood flow to the skin to activate their cooling mechanism which leaves less circulating blood to power working muscles. Children are therefore at higher risk of heat related injuries than adults. Luckily, children have a high body surface to mass ratio, which does allow them to evaporate sweat quickly (Gomes et al., 2013).
Overall, children have a high endurance capacity (like adults when adjusted for size), however, they also use a higher percentage of peak O2 uptake than their adult counterparts. Likewise, glycolytic enzyme activity is lower in children which limits their ability to sustain high intensity intervals for longer periods as glycolysis as a metabolic pathway is not as accessible (Clark et al., 2014).
It is important to note several differences in strength adaptations in children versus adults. First, most strength gains attained by pre-adolescent children stem from enhanced neuromuscular control versus muscle hypertrophy. However, these enhancements can be substantial.
In fact, children who strength training regularly can improve strength by 30-50% in just an 8-12-week time frame (Dahab & McCambridge, 2009). Additionally, when children attain increases in muscle strength, it initially supersedes the ability of the tendon to control correct range of motion. Tendon adaptation (stiffness) follows strength gains albeit more slowly than in adults (Mersmann et al., 2017).
Determining s.m.a.r.t Training Goals for kids
SMART goals (specific, measurable, attainable, realistic and timely) can be incredibly useful in the youth population. In fact, teaching goal setting and attainment strategies is highly beneficial for children as they can apply newly acquired strategies to other domains of life.
The child client should be directly involved with the creation of their training goals and should be set in terms appropriate for their level of psychological and cognitive development (Nelis et al., 2018).
Although parental involvement in goal setting is recommended, the child must direct the formation of their own goals. Fisher et al. (2018) demonstrated that the parental creation of physical activity goals did not translate to compliance from the child (Fisher et al., 2018).
movement assessments for children
Assessment drive training plans. This is true for all clients including the youngest ones. A careful medical history, sport history and questions about lifestyle should be the first portion of any assessment. Parental involvement is recommended, but the child should drive the conversation.
An overhead squat assessment (OHSA) is recommended to screen for movement compensations and muscle imbalances. Compensation patterns may differ depending on the child’s lifestyle and sport selection (active versus sedentary, sport-specific, etc).
Common imbalances seen in children are forward head position (likely underactive deep cervical flexors and an overactive upper trapezius, sternocleidomastoid and levator scapulae) and a low back arch, often the result of an anterior pelvic tilt (likely an overactive hip flexor complex and latissimus dorsi and underactive gluteus maximus, and intrinsic core stabilizers). These patterns often result from extended periods of sitting in school or playing video games or using smartphones/tablets (Clark et al., 2014).
Note that athletes will have different imbalance patterns based on their chosen sport. For instance, distance runners will often present with the low back arch compensation and oftentimes, foot flattening due to an overactive TFL with respect to the gluteus medius. In more extreme cases, a knee valgus may be noted (Arab & Nourbakhsh, 2010).
Likewise, upper body movement dysfunction may be notable in a baseball player as there may be imbalance between the external and internal rotators in the shoulder and corrective exercise to prevent a rotator cuff tear may be necessary. Pattern overloads and early sports-specialization can lead to additional movement dysfunction, so it is vital that the fitness professional take care in screening for movement compensations (Hurd & Kaufman, 2012).
Although VO2 max measurements may not be necessary, it can be helpful to screen the child’s basic cardio-respiratory condition. A YMCA 3-minute step test is a quick, easy to perform and well-validated test in assessing cardio-respiratory function in children. The results can provide useful baseline information and the test can be repeated periodically to assess for improvements (Jankowski et al., 2014).
Program Design with kids in mind
There are several key aspects in program design for younger clients.This is especially for important for sport coaches who must know the ins and outs of programming.
All exercise prescriptions for children should include a sufficient warm up (10-15 minutes), balance and flexibility, running, plyometric, SAQ and strength training components as well as a 8-12 minute cooldown period. Weekly training programs should also include sessions of aerobic exercise which can be accomplished by any activity the child enjoys.
Resistance training segments should focus on proper movement patterns and technique before weights or other resistance is added. Bodyweight exercises can be especially beneficial in this population. Resistance training should be completed 2-3 times weekly. Two sets of 10-15 repetitions of exercises incorporating all muscle groups is sufficient (Myers et al., 2017).
These ranges can fit well into a phase 1 Stabilization Endurance and, later, a phase 2 Strength Endurance training program (Clark et al., 2014). Weight selection should be determined carefully, with the child able to complete at least 10 repetitions with appropriate technique before fatigue, not failure, occurs (Myers et al., 2017)
Note that a child under the age of 13 may have a limited attention span. Changing activities quickly may be a beneficial for keeping a child’s attention. Super setting can be a useful tool when working with this population (Myers et al., 2017).
Make it Fun for the kids!
Most importantly, the fitness professional must create a fun and positive environment for their young clients and form trusting relationships. Reward systems are incredibly helpful in keeping the child motivated and accountable to their chosen goals.
Games should also be incorporated as much as possible. The fitness professional can adjust the exercise program based on the responses, attention and motivation level of their client (National Academy of Sports Medicine, 2014).
References
Ann Yelmokas McDermott, & Mernitz, H. (2013). Exercise and older patients: Prescribing guidelines. American Family Physician, 74(3), 437–444. https://www.aafp.org/afp/2006/0801/p437.html
Arab, A. M., & Nourbakhsh, M. R. (2010). The relationship between hip abductor muscle strength and iliotibial band tightness in individuals with low back pain. Chiropractic & Osteopathy, 18(1). https://doi.org/10.1186/1746-1340-18-1
Brookbush, B. (2017). Overhead Squat Assessment: Signs of Dysfunction. Brookbush Institute. https://brookbushinstitute.com/article/solutions-table-overhead-squat-assessment
Centers for Disease Control. (2019). Youth Physical Activity Guidelines. Physical Activity Guidelines for School-Aged Children and Adolescents. https://www.cdc.gov/healthyschools/physicalactivity/guidelines.htm
Clark, M. A., Lucett, S. C., & Sutton, B. (2014). NASM essentials of personal fitness training.
Burlington Jones & Bartlett Learning.
Dahab, K. S., & McCambridge, T. M. (2009). Strength training in children and adolescents: Raising the bar for young athletes? Sports Health: A Multidisciplinary Approach, 1(3), 223–226. https://doi.org/10.1177/1941738109334215
Enright, P. L., McBurnie, M. A., Bittner, V., Tracy, R. P., McNamara, R., Arnold, A., Newman,
- B., & Cardiovascular Health Study. (2003). The 6-min walk test: A quick measure of functional status in elderly adults. Chest, 123(2), 387–398. https://doi.org/10.1378/chest.123.2.387
Falk, B., & Dotan, R. (2008). Children’s thermoregulation during exercise in the heat — a revisit. Applied Physiology, Nutrition, and Metabolism, 33(2), 420–427. https://doi.org/10.1139/h07-185
Fenstermaker, K. L., Plowman, S. A., & Looney, M. A. (1992). Validation of the rockport fitness walking test in females 65 years and older. Research Quarterly for Exercise and
Sport, 63(3), 322–327. https://doi.org/10.1080/02701367.1992.10608749
Fisher, A., Hammersley, M. L., Jones, R. A., Morgan, P. J., Collins, C. E., & Okely, A. (2018).
Goal setting for weight-related behavior change in children: An exploratory
study. Nutrition and Health, 24(2), 67–74. https://doi.org/10.1177/0260106018758519 Gill, L. E., Bartels, S. J., & Batsis, J. A. (2015). Weight management in older adults. Current
Obesity Reports, 4(3), 379–388. https://doi.org/10.1007/s13679-015-0161-z Gomes, L. H. L. S., Carneiro-Júnior, M. A., & Marins, J. C. B. (2013). Thermoregulatory
responses of children exercising in a hot environment. Revista Paulista de Pediatria, 31(1), 104–110. https://doi.org/10.1590/s0103-05822013000100017
Hockings, R. L., Schmidt, D. D., & Cheung, C. W. (2013). Single-leg squats identify independent stair negotiation ability in older adults referred for a physiotherapy mobility assessment at a rural hospital. Journal of the American Geriatrics Society, 61(7), 1146– 1151. https://doi.org/10.1111/jgs.12311
Hurd, W. J., & Kaufman, K. R. (2012). Glenohumeral rotational motion and strength and baseball pitching biomechanics. Journal of Athletic Training, 47(3), 247–256. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3392154/
Jankowski, M., Niedzielska, A., Brzezinski, M., & Drabik, J. (2014). Cardiorespiratory fitness in children: A simple screening test for population studies. Pediatric Cardiology, 36(1), 27– 32. https://doi.org/10.1007/s00246-014-0960-0
Kamijo, K., Pontifex, M. B., O’Leary, K. C., Scudder, M. R., Wu, C.-T., Castelli, D. M., & Hillman, C. H. (2011). The effects of an afterschool physical activity program on working memory in preadolescent children. Developmental Science, 14(5), 1046–1058. https://doi.org/10.1111/j.1467-7687.2011.01054.x
Lazaar, N., Aucouturier, J., Ratel, S., Rance, M., Meyer, M., & Duché, P. (2007). Effect of physical activity intervention on body composition in young children: Influence of body mass index status and gender. Acta Paediatrica (Oslo, Norway : 1992), 96(9), 1315– 1320. https://doi.org/10.1111/j.1651-2227.2007.00426.x
Melton, D. I., Katula, J. A., & Mustian, K. M. (2008). The current state of personal training: An industry perspective of personal trainers in a small southeast community. Journal of Strength and Conditioning Research, 22(3), 883–889. https://doi.org/10.1519/jsc.0b013e3181660dab
Mersmann, F., Bohm, S., & Arampatzis, A. (2017). Imbalances in the development of muscle and tendon as risk factor for tendinopathies in youth athletes: A review of current evidence and concepts of prevention. Frontiers in Physiology, 8(8). https://doi.org/10.3389/fphys.2017.00987
Myers, A. M., Beam, N. W., & Fakhoury, J. D. (2017). Resistance training for children and adolescents. Translational Pediatrics, 6(3), 137–143. https://doi.org/10.21037/tp.2017.04.01
National Academy of Sports Medicine. (2014, December). Fun and Effective Group Youth Programming Strategies. Blog.Nasm.Org. https://blog.nasm.org/workout-plans/fun- effective-group-youth-programming-strategies
Nelis, S. M., Thom, J. M., Jones, I. R., Hindle, J. V., & Clare, L. (2018). Goal-setting to promote a healthier lifestyle in later life: Qualitative evaluation of the agewell trial. Clinical Gerontologist, 41(4), 335–345. https://doi.org/10.1080/07317115.2017.1416509
Powers, S. K., & Howley, E. T. (2018). Exercise physiology : theory and application to fitness and performance. Mcgraw-Hill Education.
Rikli, R. E., & Jones, C. J. (2013). Senior fitness test manual. Human Kinetics.
Roghani, T., Zavieh, M. K., Manshadi, F. D., King, N., & Katzman, W. (2017). Age-related hyperkyphosis: Update of its potential causes and clinical impacts—narrative review. Aging Clinical and Experimental Research, 29(4), 567–577. https://doi.org/10.1007/s40520-016-0617-3
Sanders, M. E. (2014). Personal balance training in focus, part II. ACSMʼs Health & Fitness Journal, 18(6), 30–35. https://doi.org/10.1249/fit.0000000000000076
Shephard, R. J. (1993). Exercise and aging: Extending independence in older
adults. Geriatrics, 48(5), 61–64. https://www.ncbi.nlm.nih.gov/pubmed/8486296